In a groundbreaking achievement for modern medicine, Qeen Biotechnologies Inc. has successfully provided bacteriophage therapy to treat a Canadian patient suffering from a periprosthetic joint infection (PJI) caused by an antimicrobial-resistant (AMR) pathogen.
This pioneering intervention demonstrates the immense potential of phage therapy as an innovative and cost-effective solution in the battle against AMR infections.
Dr Nancy Tawil, CEO and Co-founder of Qeen Biotechnologies, emphasised the significance of the achievement: “Access to phage therapy is a critical lifeline for patients battling AMR infections. At Qeen Biotechnologies, we are dedicated to ensuring that precision phage therapies are not only accessible but also scalable for widespread adoption.
“This case exemplifies our commitment to delivering innovative solutions that address one of the most pressing healthcare challenges of our time while also easing the economic burden of managing complex infections.”
What is bacteriophage therapy?
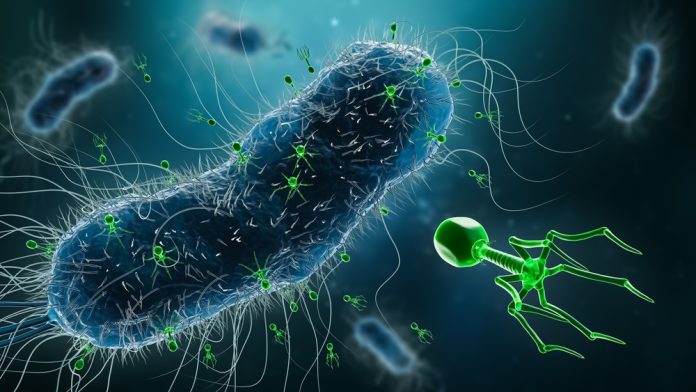
Bacteriophage therapy employs viruses known as bacteriophages to target and destroy specific bacterial pathogens.
Unlike traditional antibiotics that kill a broad spectrum of bacteria – sometimes disrupting beneficial microbes – phages are highly specific, leaving non-harmful bacteria untouched.
These naturally occurring viruses attach to bacteria, inject their genetic material, and replicate inside their host, causing the bacterial cell to burst and die.
Initially discovered over a century ago, bacteriophage therapy is experiencing a resurgence due to the alarming rise in antibiotic resistance.
Its precision and ability to combat biofilm-associated infections make it a promising alternative to antibiotics, particularly for multidrug-resistant infections.
A breakthrough in the fight against AMR
The patient was treated by Qeen Biotechnologies and received customised bacteriophage therapy under the care of Dr Stephen Vaughan.
This precision treatment was designed to tackle drug-resistant pathogens that often render traditional antibiotics ineffective.
The economic and clinical implications of this success are immense, particularly in Canada, where healthcare providers frequently grapple with limited treatment options for AMR infections.
Traditional therapies for PJIs often involve prolonged antibiotic regimens and costly two-stage revision surgeries, which can exceed $50,000 per procedure.
These methods also come with significant physical and emotional burdens for patients, including the possibility of amputation or even death when therapies fail.
Phage therapy, by contrast, offers a targeted approach that minimises the need for extended hospital stays and eliminates the reliance on exorbitantly priced antibiotics sourced from abroad.
This innovation not only enhances patient outcomes but also presents a sustainable model for healthcare systems managing the increasing prevalence of AMR infections.
Dt Vaughan added: “Instead of unlocking new research doors, we just kicked down the door. Through a tremendous team effort, including with Dr Tawil, we have been able to offer our patient an experimental treatment that previously seemed like science fiction.
“By using phage, we performed groundbreaking research that opens a new therapeutic avenue for Canadian patients with severe infections, giving hope to the most desperate.”
A call for policy support in Canada
Despite its success, bacteriophage therapy faces hurdles in adoption due to the lack of reimbursement policies for the costs associated with phage manufacturing and delivery.
Qeen Biotechnologies has called on the Canadian government to address these gaps, emphasising the urgent need for regulatory frameworks that facilitate broader access to these life-saving treatments.
This milestone underscores the transformative potential of bacteriophage therapy in addressing one of the greatest challenges of modern medicine: antimicrobial resistance.
As global healthcare systems contend with rising infection rates and limited treatment options, bacteriophage therapy emerges as a beacon of hope. Its ability to improve patient outcomes while offering significant economic advantages positions it as a sustainable solution for the future.