More than 39 million people could die from antibiotic-resistant infections in the next 25 years, according to a landmark study by the Global Research on Antimicrobial Resistance (GRAM) Project.
This comprehensive research, published in The Lancet, highlights the alarming trajectory of antimicrobial resistance (AMR) and the urgent need for global action to curb its rise.
AMR: A growing global health threat
Antimicrobial resistance occurs when bacteria and other pathogens evolve to withstand the effects of antibiotics, making standard treatments ineffective.
The new GRAM study sheds light on the increasing danger of AMR, revealing that over one million people die each year due to AMR-related infections.
If current trends continue, this number is projected to reach 1.91 million by 2050, marking a 67.5% increase from 2022.
Beyond direct deaths, AMR is also expected to play a role in 8.22 million deaths annually by mid-century – an increase of nearly 75% from 2021.
These statistics emphasise the global nature of this health crisis, with the burden of antibiotic-resistant infections rising at a troubling rate.
Age-related shifts in AMR deaths
One of the most significant findings from the GRAM study is the dramatic shift in AMR-related mortality across different age groups.
Between 1990 and 2021, deaths from antibiotic-resistant infections among children under five years old dropped by over 50%, thanks to improvements in vaccination and infection prevention measures.
However, the death toll among individuals aged 70 and older more than doubled, driven by an ageing global population and the increased susceptibility of older adults to infections.
By 2050, the study predicts that AMR-related deaths among those 70 and older will more than double, while deaths in children under five will continue to decline.
This stark contrast highlights the need for tailored interventions to protect both vulnerable age groups.
The role of pathogens
The GRAM study also delves into the pathogens responsible for the rise in antimicrobial resistance. Methicillin-resistant Staphylococcus aureus (MRSA) is a leading contributor, with global deaths caused by MRSA more than doubling from 57,200 in 1990 to 130,000 in 2021.
Additionally, Gram-negative bacteria—some of the most resistant to antibiotics—are becoming increasingly difficult to treat. Infections caused by carbapenem-resistant bacteria alone claimed 216,000 lives in 2021, up from 127,000 in 1990.
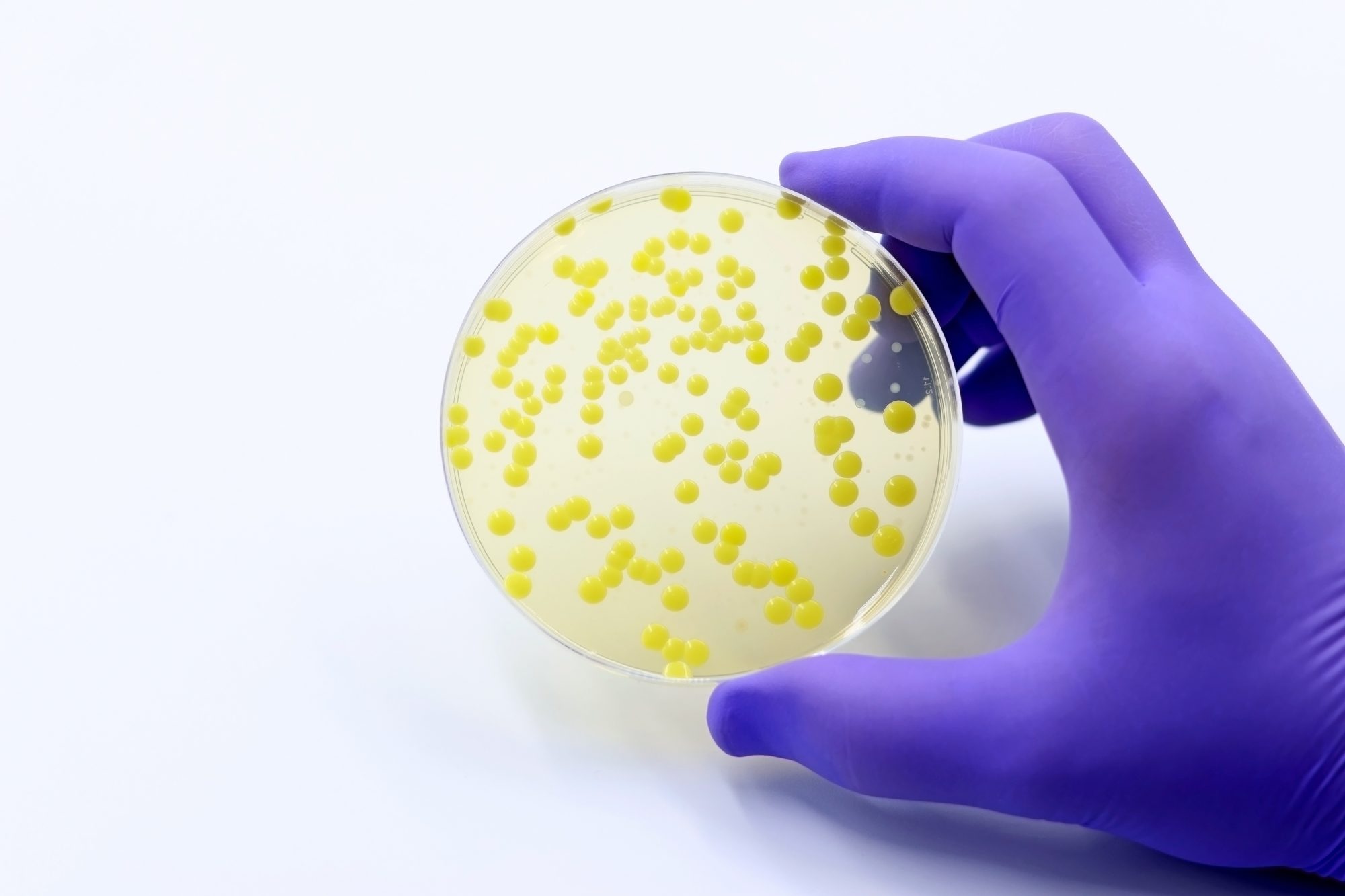
This increase in resistant pathogens underlines the importance of developing new antibiotics and treatments, especially for Gram-negative bacteria, which are notoriously difficult to combat with existing drugs.
The global impact of AMR
While antibiotic-resistant infections pose a global threat, some regions are particularly vulnerable. The GRAM study highlights five regions where deaths due to AMR rose significantly between 1990 and 2021: western sub-Saharan Africa, Tropical Latin America, high-income North America, Southeast Asia, and South Asia.
By 2050, South Asia is projected to bear the brunt of AMR-related deaths, with over 11.8 million deaths directly attributable to AMR expected between 2025 and 2050.
The regional disparities in AMR deaths underscore the need for a coordinated global response, with particular attention to regions with limited healthcare infrastructure and access to effective antibiotics.
Preventing the crisis
The GRAM study not only presents a grim forecast but also offers hope by outlining strategies to mitigate the rise of antimicrobial resistance.
The study’s authors argue that strengthening healthcare systems, improving access to antibiotics, and reducing inappropriate antibiotic use are critical steps in preventing the predicted rise in AMR deaths.
Enhancing infection prevention and control measures—such as vaccination programmes—can also play a vital role in reducing the spread of resistant infections.
Investing in research to develop new antibiotics is another key strategy. The study emphasises the urgent need for drugs targeting Gram-negative bacteria, which could prevent up to 11 million AMR-attributable deaths by 2050.
Without new treatments, the world risks losing the ability to effectively treat even common infections, reversing decades of medical progress.
The economic and social costs
Antimicrobial resistance isn’t just a public health crisis; it also poses significant economic and social challenges.
As resistant infections become harder to treat, healthcare costs are likely to soar, placing additional strain on already overburdened healthcare systems.
The loss of effective antibiotics could also lead to longer hospital stays, increased medical expenses, and a higher economic burden for families and communities.
Furthermore, the social impact of AMR is profound. Communities that are already disadvantaged are likely to bear the brunt of the crisis, particularly in low- and middle-income countries where access to healthcare is limited.
The growing number of AMR-related deaths could exacerbate existing inequalities and create new challenges in global health.
The path forward
Despite the grim outlook, experts agree that it is not too late to prevent the worst outcomes of the AMR crisis. Immediate, coordinated action can avert millions of deaths.
The GRAM study suggests that improving overall infection care and expanding access to antibiotics could save 92 million lives between 2025 and 2050.
By investing in research, improving access to antibiotics, and implementing infection control measures, we can prevent AMR from becoming an even deadlier global health crisis. The time for action is now.










