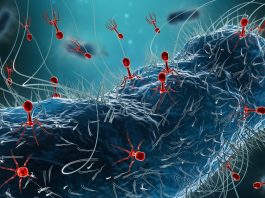
Antibiotic-resistant Salmonella is a serious public health concern that has increased recently as the bacteria has developed ways to survive drugs.
According to the U.S. Centers for Disease Control and Prevention, people can get Salmonella from eating contaminated food products or from infected people or animals — typically via unintentional contact.
A team of Penn State researchers has now discovered that household dogs are an overlooked transmission point for zoonotic pathogens that cause Salmonella. This can cause diarrhoea, fever, and abdominal cramps, and some infections can potentially have life-threatening complications.
The researchers reported that, given dogs’ proximity to humans and the use of critically important antibiotics in companion animal medicine, household dogs represent a risk for the spread of antimicrobial-resistant Salmonella.
They found that better awareness of the risk and proper hygiene could potentially help mitigate cross-species infections.
How dogs spread antimicrobial-resistant Salmonella
Salmonella infections in dogs can be clinical — showing signs or symptoms — or asymptomatic, with numerous studies reporting Salmonella isolation from clinically healthy dogs, according to team leader Erika Ganda.
She explained that a major concern is the closeness of humans and pet dogs, which creates ample opportunity for Salmonella ‘zoonosis’ — the disease transmitted to humans from animals.
Furthermore, pet-management decisions involving food contamination, improper food handling or both can increase the likelihood of infection.
Investigating strains spread from dogs
To investigate antimicrobial-resistant Salmonella and the zoonotic potential of nontyphoidal Salmonella isolated from dogs and humans, the researchers leveraged existing biosurveillance infrastructure.
Using the U.S. Food & Drug Administration’s Veterinary Laboratory Investigation and Response Network, they identified all nontyphoidal Salmonella strains isolated from domestic dogs between May 2017 and March 2023.
Then, they matched the timing and location of those 87 cases to strains isolated from humans in the National Center for Biotechnology Information database maintained by the National Library of Medicine at the National Institutes of Health, which provides access to biomedical and genomic information.
They found 77 suspected zoonotic cases — meaning the bacteria moved from a pet dog to a human — comprising 164 strains collected from 17 states in the United States.
Strains of antimicrobial-resistant Salmonella isolated from dogs included diverse serovars or distinct variations within the species of bacteria, with most being clinically relevant to human health.
While the datasets did not contain information on the severity of infection or treatments, the researchers did find that all identified strains possessed antimicrobial resistance genes for drug classes deemed critically or highly important by the World Health Organization.
“We identified 16 nontyphoidal Salmonella isolates from humans closely related to more than one of six dog-associated strains,” said Sophia Kenney, a student in the molecular, cellular and integrative biosciences doctoral program at Penn State.
“Collectively, our data emphasises the importance of antimicrobial stewardship and sustained biosurveillance beyond human and agriculture-associated veterinary medicine, using a ‘One Health’ framework that accounts for all transmission points — including companion animals.
Advancing stewardship within the One Health model
Antimicrobial stewardship in companion animal veterinary medicine is crucial for mitigating antimicrobial resistance within the One Health model.
“We have this close bond with companion animals in general, and we have a really close interface with dogs,” Kenney explained.
“So, we asked the question: What’s the role of companion animals in transmitting zoonotic diseases like Salmonella, since they can get it? Salmonella infections in dogs are uncommon, but we’re aware of foodborne outbreaks related to pet treats, contact with contaminated pet food, and improper food handling.”
The researchers also pointed to an outbreak of antimicrobial-resistant Salmonella infections in people linked to pig ear pet treats in the United States a few years ago that sickened 154 people across 34 states.
This highlights that simple hygiene practices such as hand washing are needed to protect both our pets and ourselves.