Dr Martin Stauber, CEO of GratXray AG, describes the company’s new one-stop solution for accurate and painless breast cancer diagnosis.
Breast cancer is by far the most common cancer in women.1 The World Health Organization (WHO) has estimated that 2.1 million new cases of breast cancer were diagnosed in 2018, with 627,000 women dying from it.2 In other words, one in nine women will develop breast cancer during their lifetime, and one in four will die from this disease. Current forecasts and statistics indicate a significant rise of both incidences of breast cancer and associated mortality. It is predicted that worldwide incidences will reach approximately 3.2 million new cases by 2050;1 with the increase in costs that this entails. These figures reflect the magnitude of the problem, its impact on society, and the need for action to reduce its impact.
To reduce the mortality rate, cut hospital costs, and lower social burden, early and accurate detection is essential. Growth of 1mm in tumour diameter increases the risk of death by 1%.3 For this reason, screening programmes have been established in many countries. However, breast cancer screening is controversially discussed in many regions, since mammography, the only method currently approved for breast cancer screening, has severe limitations. In Germany, for instance, only 50% of the women receiving an invitation for breast cancer screening participate in the programme.4 Thus, many tumours are missed only because women fear the pain or doubt the benefits of screening. Therefore, breast radiologists worldwide are calling for new methods with significantly enhanced tissue sensitivity and specificity under dose control.
Modalities and limitations
If a screening result was found to be suspicious or if a woman decides to do a preventive checkup, they will all end up in a diagnostic setting. There, several imaging modalities are combined to get to an image-based diagnostic result. In most cases, tomosynthesis or mammography are combined with ultrasound (US) and, in fewer cases, even with magnetic resonance imaging (MRI). There is no single medical device able to assess all clinically relevant information for an accurate diagnosis.
The combination of these imaging modalities is time-consuming, requires an experienced operator, and an expensive machinery park. If the image-based diagnostic result is found to be suspicious, a tissue biopsy is taken to confirm the result. However, in Germany it was reported that only 50% of all biopsies were positive.4 This shows the overall limitation of the state-of-the-art imaging approach and the need for improved methods.
The solution
GratXray is developing a disruptive medical device for accurate, reliable, and painless breast cancer diagnosis that will cut costs on the pathway of breast cancer care. This new device integrates a dedicated breast computed-tomography (BCT) system with grating interferometry (GI), a high-contrast X-ray imaging method for soft tissue.
Computed Tomography (CT) is an X-ray based imaging technique to acquire true 3D images of the internal structure of the body. A set of X-ray images acquired from different angles around the body is mathematically reconstructed into a 3D image. An inherent advantage of this technology is, that the breast can be measured in its natural state without compression. Furthermore, a 3D image allows the radiologists to virtually scroll through the breast tissue. Thus, the tissue-overlap problem, which is a severe limitation of mammography, especially in women with dense breast tissue, can be overcome. GratXray will use a spiral CT configuration which can deliver isotropic spatial resolution and uniform dose distribution, which is crucial for the diagnostic accuracy and for the patient dose management.5
Grating Interferometry (GI)
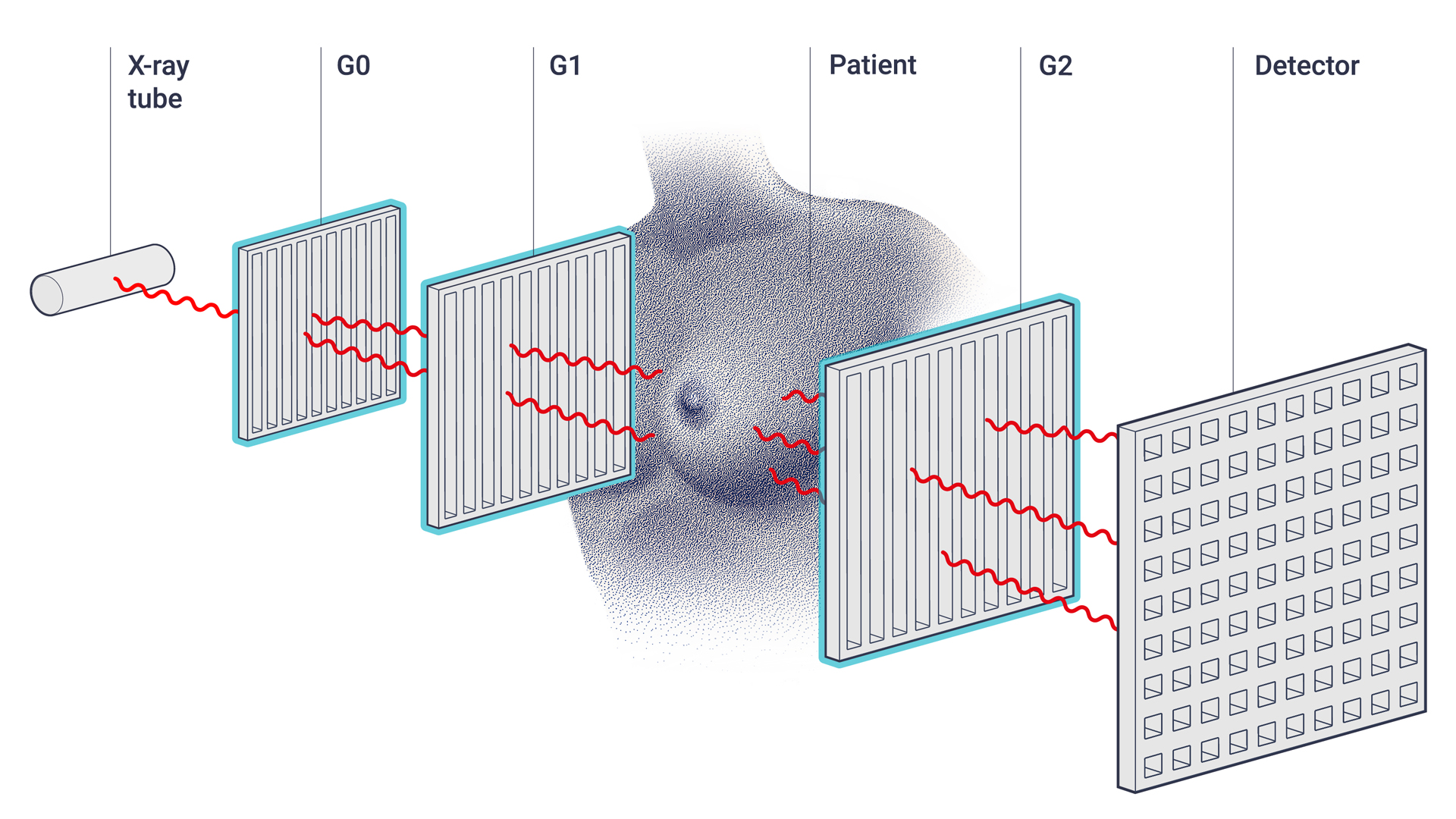
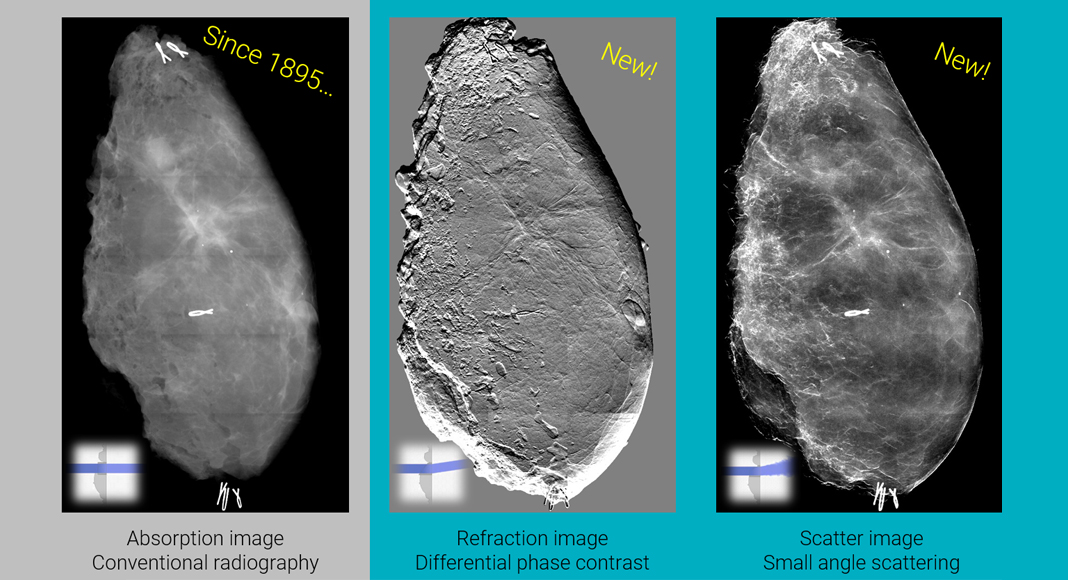
Grating Interferometry (GI) is a cutting-edge imaging technique that has the potential to revolutionise medical imaging.6 A grating interferometer is an X-ray system with three additional optical components, the gratings (see Fig. 1). It records three complementary signals simultaneously in a single acquisition: the conventional absorption image, the differential phase contrast image, (refraction image) and the scattering image (see Fig. 2). The latter two have so far been considered as noise sources. Grating interferometry actually makes use of those additional signals to improve diagnostic contents, thereby opening new opportunities for medical imaging.
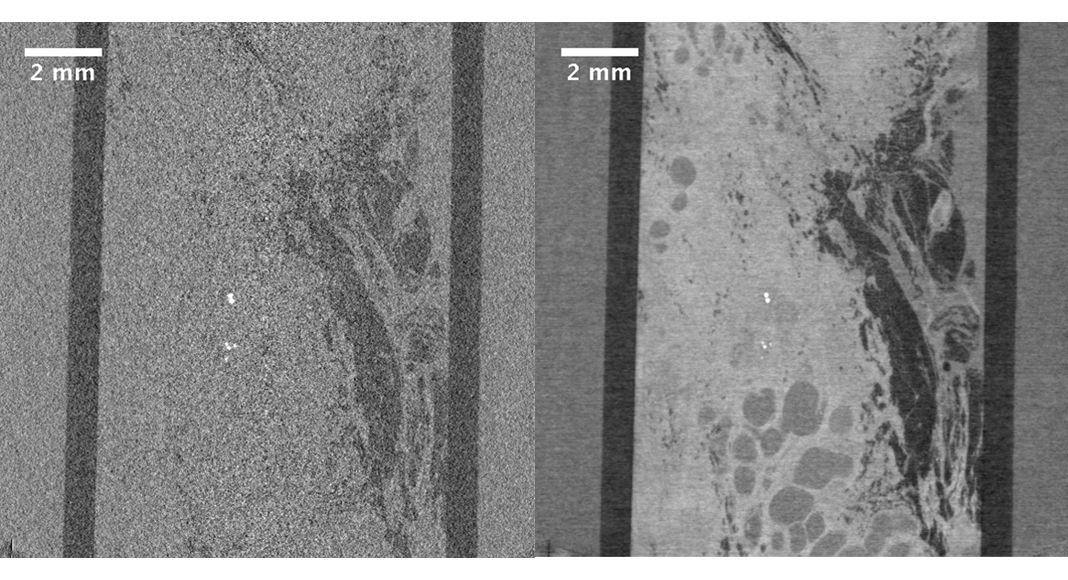
For breast tissue, the phase contrast signal is significantly larger than the absorption signal in the medical energy range. Therefore, at the same dose, the image quality of phase contrast will be substantially better than absorption contrast; or, in order to obtain the same image quality, the dose can be reduced. Fig. 3 shows a direct comparison of a slice taken through a 3D dataset of a human breast biopsy tissue acquired on a lab micro-computed tomography system, with and without GI. Whereas in the conventional CT image the different tissue types cannot be separated from each other, they are clearly distinguishable in the GI enhanced CT image.
The method was proven on several lab instruments and its power and potential for biomedical imaging has recently been demonstrated by scanning mouse embryos and the human left ventricle.7 Moreover, a commercial mammography system was retrofitted with GI,8 and the system has been installed at the University Hospital in Zürich, to run a first clinical trial in spring 2021.
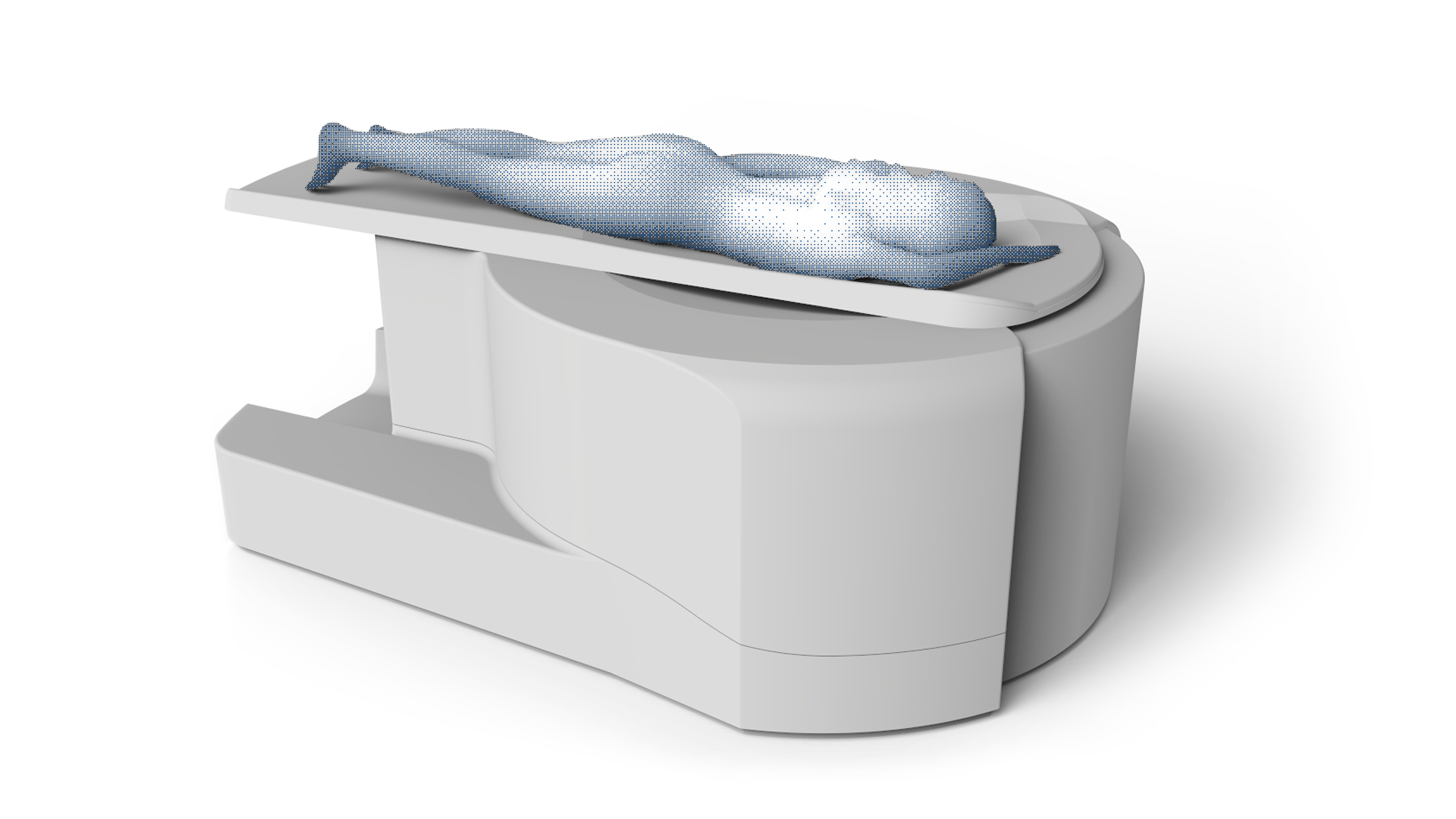
At GratXray, we are taking the next step by integrating GI in a dedicated breast computed-tomography (GI-BCT) system (see Fig. 4). The women will lay prone on the patient bed and the breast will be measured in the breast position aperture without any compression. Unlike any other competitor, our GI-BCT system not only integrates all the strengths of existing technologies in a single multi-modality device, but thanks to its technology based on grating interferometry it also provides additional capacities and advantages, which yields many advantages for women, clinicians, hospitals, and society.
Benefits
The main beneficiaries will be women who receive a painless and accurate breast cancer diagnosis without the need for breast compression. A major limitation of mammography is imaging women with dense breast tissue, which causes many tumours to be missed. Thanks to the high-contrast 3D images of GI-BCT, diagnosis becomes largely independent of tissue density. This allows tumours to be detected at a much earlier stage, enabling less invasive treatment and increasing survival rates.
With GI-BCT, radiologists can base their diagnoses on more comprehensive information while saving a lot of time. Improved soft tissue discrimination with more specific lesion visibility combined with true 3D distribution of microcalcifications makes this system a complete solution for breast cancer imaging. Workflow is optimised as imaging is reduced to a single device, saving costs and time. It has been estimated that the time required with the GratXray system is one-third compared to a standard diagnostic setup of mammography and ultrasound, not including MRI. Thus, three times as many women can be diagnosed in the same amount of time and the equipment can be optimally utilised.
The improved workflow and more women-friendly breast cancer diagnosis allow hospitals to attract more women, which is associated with increased revenue. By using GratXray’s GI-BCT, hospitals can also differentiate themselves from their competition and distinguish themselves as an innovative player. In addition, they can downsize their machinery park, saving on costs for premises, equipment, and maintenance.
Women are obviously the main beneficiaries of GratXray’s new technology, but this also results in an enormous benefit for society as a whole. The social burden and indirect costs associated with breast cancer can be significantly reduced with the early detection of breast cancer, as treatment is less invasive and burdensome for the women concerned.
State of development
In 2017, GratXray was founded as an ETH (Swiss Federal Institute of Technology) and PSI (Paul Scherrer Institute, Switzerland) spin-off to bring the new high-contrast X-ray method to market. The method has been pioneered for more than a decade by Professor Marco Stampanoni and his group and is protected by a solid patent portfolio. GratXray has exclusive access to this portfolio and will develop medical devices based on this disruptive technology.
This new method will bring great benefits where classic X-ray systems fail or provide unsatisfying results. There are many applications that will profit from this new technology. However, as a young start-up company, GratXray needs to focus on one application, and the founders therefore decided to set the first focus on breast cancer diagnosis. The new method perfectly fits this application and there is a significant need for improved methods in this field. This strategy was verified and optimised through interviews with women, radiologists, radiology nurses, and other health-tech professionals. In 2017, this strategy was awarded the Swiss Technology Award, the most important prize for innovation in Switzerland. Here, the jury rated the benefits for women and society as very high.
After this initial success, GratXray quickly attracted its first convertible loans from business angels to launch operations. It was clear from the outset that the capital required to develop and certify this product would be relatively high. For this reason, GratXray evaluated various financing scenarios during the early stages and ultimately decided to work closely with its parent institute, PSI. This close collaboration allowed GratXray to benefit greatly from PSI’s expertise in the development of high-tech devices and its university environment. A first version of the functional prototype was completed in January 2021.
After this successful development, GratXray is now in the process of becoming more independent from the university environment in order to tackle the next steps: the construction and certification of the medical device. In this phase, the company needs additional capital, which opens the opportunity for new investors to join GratXray’s exciting journey.
Future opportunities
With GratXray’s GI-BCT device, all clinically relevant features for diagnosing breast cancer are collected in one single image for the first time. Therefore, this new device is the first one-stop solution for accurate and painless breast cancer diagnosis, having the potential to become a new gold standard in breast cancer imaging.
Breast cancer imaging is just the first application, and GratXray plans to develop new medical devices for other applications based on its innovative high-contrast X-ray imaging platform. Wherever soft tissue contrast needs to be increased in X-ray imaging, this platform is proving to be the method of choice. These new applications include, for example:
- Pulmonary radiography, where the new contrasts allow the earlier diagnosis of lung cancer and the quantitative diagnosis of asymptomatic and symptomatic respiratory virus infections in pandemic situations such as MERS, SARS, COVID-19, and whatever the future may hold;
- Head CT scans, speeding up brain imaging as compared to MRI;
- Joint imaging systems, providing better diagnosis of cartilage damage or tendon ruptures; and
- Whole-body CT scans, allowing for imaging of any part of the body with very high soft tissue contrast at a high image resolution.
References
1 Z. Tao, A. Shi, C. Lu, T. Song, Z. Zhang, and J. Zhao, ‘Breast Cancer: Epidemiology and Etiology’, Cell Biochem. Biophys., vol. 72, no. 2, pp. 333–8, Jun. 2015
2 F. Bray, J. Ferlay, I. Soerjomataram, R. L. Siegel, L. A. Torre, and A. Jemal, ‘Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries’, CA. Cancer J. Clin., vol. 68, no. 6, pp. 394–424, Nov. 2018
3 J. S. Michaelson et al., ‘The Effect of Tumor Size and Lymph Node Status on Breast Carcinoma Lethality’, Cancer, vol. 98, no. 10, pp. 2133–2143, 2003
4 D. Mammographie Screening Programme, ‘Jahresbericht Evaluation 2017,’ 2017
5 W. A. Kalender, M. Beister, J. M. Boone, D. Kolditz, S. V Vollmar, and M. C. C. Weigel, ‘High-resolution spiral CT of the breast at very low dose: concept and feasibility considerations’, Eur. Radiol., vol. 22, no. 1, pp. 1–8, Jan. 2012
6 T. Weitkamp et al., ‘X-ray phase imaging with a grating interferometer’, Opt. Express, vol. 13, no. 16, pp. 6296–304, Aug. 2005
7 J. Vila-Comamala et al., ‘High Sensitivity X-ray Phase Contrast Imaging by Laboratory Grating-based Interferometry at High Talbot Order Geometry’, Opt. Express, vol. 29, no. 2, pp. 2049–2064, Dec. 2021
8 C. Arboleda et al., ‘Towards clinical grating-interferometry mammography’, Eur. Radiol., vol. 30, no. 3, pp. 1419–1425, Mar. 2020
Please note, this article will also appear in the fifth edition of our quarterly publication.









