BAT explains how they are working to promote a clear and transparent landscape for research on E-cigarettes.
Millions of people around the world are using electronic cigarettes (ECs). In the UK alone, around three million people are believed to be using vapour products, which is a significant increase on the 500,000 that were using these products in 2012. This vapour revolution can partly be attributed to the fact that the new devices provide many of the effects smokers get from conventional cigarettes — namely sensory, ritual and nicotine effects.
Electronic cigarettes are electrical products that heat a liquid known as an e-liquid, typically comprising of glycerol, propylene and water, which in most cases contain flavours and nicotine, to create a vapour that can be inhaled. The liquid is heated via a ‘coil and wick’ system, similar to that of an oil lamp. ECs have a cotton wick that draws the e-liquid up from a reservoir. A metal coil is wrapped around the wick, and when power is passed across the coil the e-liquid is turned into a vapour aerosol. This simple technology has supported the growth of this remarkable industry, and generally works well. One drawback of poorly designed coil-and-wick ECs is if the cotton wick runs dry – this can lead to something called ‘dry wicking’, which can thermally degrade the e-liquid, producing some of the combustion toxicants typically associated with cigarette smoke.
Cigarette smoke: the technical challenge
We previously outlined a scientific framework to assess the risk profile of ECs relative to cigarettes. Conventional cigarettes contain tobacco which when lit and puffed by smokers, combusts at temperatures of more than 950°C to form smoke. This smoke contains more than 6,500 individual compounds, of which around 100-150 are known as toxicants. Long-term exposure to these toxicants can cause diseases such as cardiovascular disease, lung diseases and cancer. Several public health bodies have stated that it is the exposure to these toxicants in smoke which cause diseases, not nicotine.
Electronic cigarettes: The technical solution?
In the UK, it has been reported that since 2013, three million people have used electronic cigarettes. The operating temperature of ECs sits at around 250°C, much lower than combustion at 950°C. As the devices do not contain tobacco and operate at substantially lower temperatures, they have the potential to produce aerosols with substantially reduced levels of toxicants relative to cigarette smoke.
David O’Reilly, Group Scientific and R&D Director for BAT, said: “We recognise the power of technology and the fact that our consumers, like all modern consumers, want safe and satisfying solutions for their every need. We have fully engaged with the challenges this presents and transformed our R&D from one focused on a single plant-based product – the cigarette – to one focused on delivering multi-category consumer electronic-based offerings.”
Our approach
The potential benefits of tobacco harm reduction for public health are enormous, and at present ECs need a balanced and transparent scientific debate to support substantiation of their potential to play a role in tobacco harm reduction. At BAT, we have adopted an open and transparent approach to the science we conduct on electronic cigarettes. We have published more than 200 scientific papers, across all categories of the risk continuum including electronic cigarettes, in peer-reviewed scientific journals in the past five years across multiple scientific disciplines, and using a range of methodologies.
We recently summarised published work on one of our electronic cigarettes (Murphy, 2017), describing data from pre-clinical safety evaluations and setting out scientific evidence to support substantiation of the potentially reduced-risk nature of ECs. Other tobacco companies are also publishing their data on electronic cigarettes. In March 2017, several major tobacco companies shared their latest research findings on ECs at the Society for Research in Nicotine and Tobacco (SRNT) meeting in Florence, Italy, a leading conference for US public health stakeholders. These activities are further signals of intent from EC manufacturers, including ourselves, that they are committed to publishing their studies and results, and desire open, transparent and robust debate about them.
Last year, we published the findings from our pharmacokinetic (PK) studies on ECs (Fearon, 2017). These studies were approved by the appropriate independent ethics boards and carried out following Good Clinical Practice guidelines of the International Convention for Harmonisation (ICH). We also registered (on ISRTCN.com) the protocols ahead of the study commencement to ensure transparency of the study objectives and measured endpoints. Registering trials in this manner also forms a commitment to publish the results from the studies, irrespective of the findings. BAT follows recognised standards, uses validated methods where possible, and publishes the findings in peer-reviewed journals. In conducting our studies in this way, we support the development of robust data that will withstand scrutiny.
Regulatory outlook
ECs have not been around long enough to determine potential long-term health risks but scientists are working at pace to identify potential benefits, as well as risks and ways to mitigate them. After reviewing scientific literature, Public Health England (PHE; McNeill, 2018) and the Royal College of Physicians (RCP, 2016) published reports concluding that ECs could be around 95% less harmful than smoking cigarettes. In the UK, ECs are regulated by the Medicines and Healthcare Regulatory Agency (MHRA) within the Department of Health.
Scientific input from a range of stakeholders is required to strengthen policy; this should include industry, as companies are major funders of research and development, and the industry has good science to contribute. The American Chemical Society (ACS) strongly supports the use of insightful, comprehensive, scientific input into the development and evaluation of policy options, and encourages scientific integrity policies that help integrate scientific assessments into governmental policy development and implementation (ACS, 2014).
The ACS recommends that federal agencies should consistently review how they obtain unbiased scientific and technical input for policy development. Scientific and technical advisory committees ought to be composed of qualified scientists and technical experts. Some of this expertise could be provided by the industry, as long as the scientific information and the frameworks created to evaluate and use the information are timely and presented transparently. Such an approach would not be without precedent; in the late 1980s an initiative beginning in the European Community and expanding into Japan and the USA saw a joint regulatory–industry collaboration develop what is now the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). The original harmonisation addressed three major areas as the basis for approving and authorizing new medicines:
- Safety;
- Quality; and
- Efficacy.
The success of the ICH in improving drug regulatory standards is attributed not only to a process of scientific consensus developed between industry and regulatory experts, but also to the commitment of the regulatory parties to implement the ICH Tripartite Harmonised Guidelines and recommendations (see:http://www.ich.org/about/history.html).
We were the first major tobacco company to launch a vapour product (July 2013) and have developed a product stewardship approach for ECs, making several key learnings to continue to improve the safety profile of our products.
Guided by the European Union TPD, the UK regulator has developed a set of requirements aimed at controlling the safety and quality of electronic cigarettes and the liquids used in them. These include banning certain additives, including stimulant compounds such as caffeine, as well as making packaging child resistant and tamper evident. Regulations and standards in this area are still evolving.
Sandra Costigan, Principal Toxicologist for vapour products at BAT, said: “It’s not known where the vast majority of products out there sit scientifically – better oversight is needed to protect consumers in the long term. To make sure that consumers are not exposed to anything at a level that could pose an unacceptable hazard, we go above and beyond what is legally required to consider products as acceptable.”
Although ECs do not traditionally contain tobacco, they can contain some toxicants in the vapour emissions. This can be minimised through responsible and effective product stewardship. We carry out scientific studies before we launch our products, and our three-step product stewardship process helps us to remove many potential hazards from our ECs. The first step is to ensure that every ingredient is scrutinised from a toxicological perspective and that no ingredients that are known Carcinogens, Mutagens or Reproductive toxicants (CMRs) are included in e-liquid recipes (Costigan, 2015). We also screen for potential respiratory sensitisers (Costigan, 2017). Secondly, the device materials are tested to ensure they do not release toxicants into the aerosol emissions through extraction during use, that the battery conforms to all regulatory safety requirements and that charging and discharging safety features are included in the microchip design. Finally, the emissions of the EC are tested to assess the levels of toxicants, comparing them to ECs previously internally approved for launch.
We have also publicly shared other key findings from our product stewardship process. For example, most manufacturers now prohibit the use of diacetyl in e-liquids (as diacetyl has been linked to impairment of lung function). We discovered that diacetoin can be a precursor to diacetyl, so we also prohibit the use of this in our e-liquids. We also discovered that some acids (e.g. citric acid) can form anhydrides that are respiratory sensitisers when heated during vapourisation in ECs. We have shared our findings so other manufacturers can learn from our studies.
Flavour is hugely important to EC users, and although some flavourings are known to cause allergic reactions, there are no regulatory-related restrictions regarding their use. Many smaller companies are unable to employ toxicologists due to their budgets, or have the expertise to carry out toxicological risk assessments on their e-liquids. To help, and having already published our view on the responsible use of flavours in vaping products, we devised and published the first practical guide for the allergy-safe use of e-liquid ingredients, including flavours.
Costigan said: “As NGPs evolve, we are continuing to adopt new approaches to ensure our robust stewardship continues. It’s a big challenge, but we are well focused on ensuring we put the best products on the market in terms of safety – and consumer appeal – to give smokers the confidence to try to switch to our NGPs.”
Around the world
Countries including Japan, Australia, Malaysia, New Zealand, and Brazil have banned the sale of ECs, while others such as Cambodia, Jordan, Nepal and Panama, have banned their consumption, which has led in some cases to the formation of EC ‘black markets’.
However, New Zealand completely reversed its position on electronic cigarettes in 2017, and their new policies are similar to those in the UK. The situation differed in Canada, where nicotine-containing electronic cigarettes were initially banned; recently the scientific evidence was reviewed at the request of the government, and new EC-specific legislation was approved that will permit the sale of ECs. In light of the growing evidence regarding Next Generation Products, other governments may change their position and provide regulatory support of these products.
Today, the USA is the largest EC market in the world, with more than 11.5 million people reported as regular users. This market was a remarkable consumer-driven phenomenon that developed quickly, with a great deal of fast-paced innovation. The EC regulatory journey is still evolving alongside a relatively young regulatory approach to tobacco products. The Family Smoking Prevention and Tobacco Control Act (FSPTCA), which created the FDA’s Center for Tobacco Products (CTP), was only signed into law in June 2009. Despite the fact that electronic cigarettes typically contain medical-grade nicotine and no tobacco, in the USA the FDA has deemed them ‘tobacco products’ and they are to be regulated by many of the same rules that apply to tobacco products, such as cigarettes. A key part of the FDA’s regulatory approach is the Pre-Market Tobacco Approval (PMTA) process, which was outlined in the ‘deeming regulations’ for ECs issued in July 2016. This means that for any product that was not already on the market before 15 February 2007, the manufacturer will need to submit a PMTA to remain on the market.
What this may mean in practice is that a dossier of preclinical, clinical and population studies must be compiled and submitted to the FDA CTP. Each dossier could cost up to £15m (~€168.m) and take three years to complete the studies and pull together the documentation. There are real fears that this could – at worst – put the majority of EC companies out of business, as they would be unable to fund this regulatory process for their product portfolios or – at best – slow the innovation cycle of products to the extent that the US market would be, to all intents and purposes, frozen. This may unduly restrict consumers’ access to products that may potentially facilitate their complete switch from smoking.
Rapid evolution
The pace of innovation in this novel area is incredibly fast. For the regulatory process to work, it would require a bridging process, where data from the first-generation product could be added to on a ‘needs’ basis, to enable the regulatory authorisation to be transferred to the second generation.
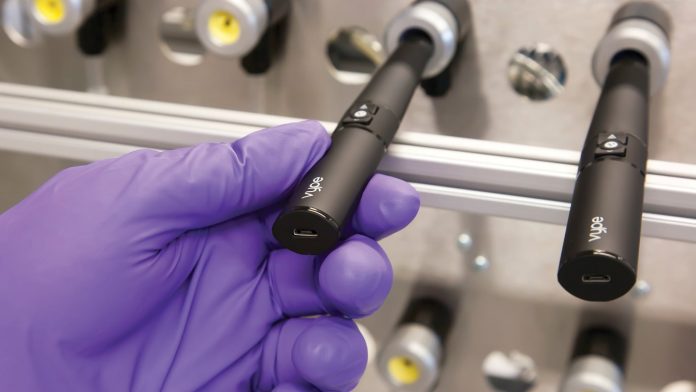
James Murphy, Head of Reduced Risk Substantiation at BAT, said: “The series of studies can take up to five years to complete — much longer than the typical three to six-month innovation cycle of an EC. While still compiling the data dossier for our first Vype ePen, for example, we launched a new, improved version of the product and had also begun work on revamping that one!”
Scientific assessment of ECs
We recently published a series of 20 scientific peer reviewed papers on a closed modular EC summarising the reduced levels of harmful chemicals in the EC emissions relative to cigarette smoke (Margham, 2016). We also showed that the EC emissions elicited substantially reduced toxicological responses in a series of traditional (Thorne, 2017) and 21st century toxicological tests (Banerjee, 2017). In the UK, on the basis of more than 200 studies on ECs, several public health authorities have supported ECs as potentially less risky products than smoking.
Professor Kevin Fenton, Director of Health and Wellbeing at Public Health England, said: “Smoking remains England’s number one killer and the best thing a smoker can do is to quit completely, now and forever. E-cigarettes are not completely risk free but when compared to smoking, evidence shows they carry just a fraction of the harm. The problem is people increasingly think they are at least as harmful and this may be keeping millions of smokers from quitting. Local stop smoking services should look to support e-cigarette users in their journey to quitting completely,” (see:https://www.gov.uk/government/news/e-cigarettes-around-95-less-harmful-than-tobacco-estimates-landmark-review).
A report from the Royal College of Physicians (RCP), entitled ‘Nicotine without smoke: tobacco harm reduction’, concluded that electronic cigarettes are likely to be beneficial to the UK public’s health. Professor John Britton, chair of the RCP’s Tobacco Advisory Group, said: “The growing use of electronic cigarettes as a substitute for tobacco smoking has been a topic of great controversy, with much speculation over their potential risks and benefits. This report lays to rest almost all of the concerns over these products, and concludes that, with sensible regulation, electronic cigarettes have the potential to make a major contribution towards preventing the premature death, disease and social inequalities in health that smoking currently causes in the UK. Smokers should be reassured that these products can help them quit all tobacco use forever,”
(see:https://www.rcplondon.ac.uk/news/promote-e-cigarettes-widely-substitute-smoking-says-new-rcp-report).
Clinical assessments of electronic cigarettes
Several studies have demonstrated that smokers who exclusively switch to electronic cigarettes can reduce their exposure to certain harmful chemicals (Shahab, 2017). We are currently in pre-launch assessment of a novel type of EC, which uses a novel sintered plate (EC-P) as the vaporisation technology in lieu of the ‘coil and wick’ technology that exists in the majority of ECs marketed today. The plate-based model has even lower levels of certain toxicants in its emissions than the corresponding ‘coil and wick’ electronic cigarettes. The plate technology was invented by Helmut Buchberger, an Austrian engineer who now works closely with BAT. Buchberger said: “It’s only through this collaboration that my invention has become a disruptive piece of technology that is set to revolutionise vaping and transform the industry.”
We conducted a clinical study in the UK (ISRCTN80651909) to assess if smokers who switch to EC with the EC-P technology would be exposed to reduced levels of toxicants (McEwan, 2017). The Institute of Medicine (IOM) published its guidelines on standards for modified risk tobacco products (IOM 2012) and stated that these products should have the same responses in testing to smoking cessation. Therefore, in our clinical study design we recruited 150 smokers to a UK clinic for seven days. For the first two days all 150 subjects continued smoking and blood, breath and urine samples were taken every 24 hours. On day three, the subjects were split into three cohorts of 50 subjects. The first cohort continued smoking for the remaining five days, the second cohort switched to using the EC-P version exclusively and the final cohort stopped all tobacco product use.
Smokers who continued smoking maintained their elevated levels of carbon monoxide (CO) and nicotine-derived nitrosamine ketone (NNK) for the duration of the study. Those who switched to the E-CP version exclusively had rapid reduction in biomarker levels of CO and NNK, which were maintained at substantially reduced levels for the duration of study. Smokers who stopped all tobacco product use had rapid reduction in certain biomarker levels of CO and NNK, which were maintained at substantially reduced levels for the duration of study.
In the majority of cases, subjects who switched exclusively to the EC-P version had similar reductions in biomarkers to the cessation group. From these studies, we concluded that by exclusively switching to the EC-P version, smokers could reduce their exposure to some harmful chemicals. In many cases, these biomarker reductions were of the same magnitude as smoking cessation.
Expanding scientific approaches
Over the past couple of years, we have expanded our scientific approaches to look at other potential benefits of Next Generation Products. Areas of interest include the reduced impact on air quality and improved oral hygiene when compared to smoking cigarettes. We are also exploring various methods for post-market surveillance and population modelling of the potential long-term effects of our ECs.
Chris Proctor, BAT’s Chief Scientific Officer, said: “It is an exciting scientific programme with the potential of making a real difference to public health. But I am very conscious that there remains suspicion of manufacturers’ data acquired on their own products, and that this is multiplied in the case of tobacco. That is why we need to publish in peer-reviewed journals and be active in scientific societies and present our data. Science is essentially a collaborative effort, and we continue to seek partnerships to advance our science.”
Looking to the future
In the dynamic world of ECs, products are rapidly improving to meet smokers’ needs. Consumers require access to accurate information to help them access products that are effective and potentially less risky. Data we have generated on ECs illustrates their potential as reduced risk products, in line with statements from several UK public health authorities. We are conducting longer-term clinical studies to assess if the reduction in exposure to harmful chemicals by switching from smoking to exclusive EC use translates into a reduction in risk for smoking-relating diseases.
References
Murphy, J., Gaca, M., Lowe, F., Minet, E., Breheny, D., Prasad, K., Camacho, O., Fearon, I.M., Liu, C., Wright, C. and McAdam, K., 2017. ‘Assessing modified risk tobacco and nicotine products: Description of the scientific framework and assessment of a closed modular electronic cigarette’. Regulatory Toxicology and Pharmacology, 90, pp.342-357.
Fearon, I.M., Nides, M., Eldridge, A., Camacho, O.M., Murphy, J. and Proctor, C.J., 2017. ‘A pharmacokinetic study to examine nicotine delivery from e cigarettes and a conventional cigarette in healthy subjects during a brief period of ad libitum use’. International Journal of Clinical Trials, 4 (4), pp.131-138.
McNeill, A., Brose, L.S., Calder, R., Bauld, L. and Robson, D., 2018. ‘Evidence review of e-cigarettes and heated tobacco products 2018’. A report commissioned by Public Health England. London:
Royal College of Physicians, 2016, July. ‘Nicotine without smoke: tobacco harm reduction’. London: RCP.
American Chemical Society, 2017. ‘Scientific Integrity in Public Policy’. Available at: https://www.acs.org/content/acs/en/policy/publicpolicies/sciencepolicy/scientificintegrity.html
Costigan, S. and Meredith, C., 2015. ‘An approach to ingredient screening and toxicological risk assessment of flavours in e-liquids’. Regulatory Toxicology and Pharmacology, 72 (2), pp.361-369.
Costigan, S. and Lopez-Belmonte, J., 2017. ‘An approach to allergy risk assessments for e-liquid ingredients’. Regulatory Toxicology and Pharmacology, 87, pp.1-8.
Margham, J., McAdam, K., Forster, M., Liu, C., Wright, C., Mariner, D. and Proctor, C., 2016. ‘Chemical composition of aerosol from an e-cigarette: a quantitative comparison with cigarette smoke’. Chemical Research in Toxicology, 29 (10), pp.1662-1678.
Thorne, D., Larard, S., Baxter, A., Meredith, C. and Gac¸a, M., 2017. ‘The comparative in vitro assessment of e-cigarette and cigarette smoke aerosols using the γH2AX assay and applied dose measurements’. Toxicology Letters, 265, pp.170-178.
Banerjee, A., Haswell, L.E., Baxter, A., Parmar, A., Azzopardi, D., Corke, S., Thorne, D., Adamson, J., Mushonganono, J., Gaca, M.D. and Minet, E., 2017. ‘Differential Gene Expression Using RNA Sequencing Profiling in a Reconstituted Airway Epithelium Exposed to Conventional Cigarette Smoke or Electronic Cigarette Aerosols’. Applied In Vitro Toxicology, 3 (1), pp.84-98.
Public Health England, 2015, Press Release ‘E-cigarettes around 95% less harmful than tobacco estimates landmark review’. Available at: https://www.gov.uk/government/news/e-cigarettes-around-95-less-harmful-than-tobacco-estimates-landmark-review
Royal College of Physicians, 2016, Press Release ‘Promote e-cigarettes widely as substitute for smoking says new RCP report’. Available at: https://www.rcplondon.ac.uk/news/promote-e-cigarettes-widely-substitute-smoking-says-new-rcp-report
Shahab, L., Goniewicz, M.L., Blount, B.C., Brown, J., McNeill, A., Alwis, K.U., Feng, J., Wang, L. and West, R., 2017. ‘Nicotine, carcinogen, and toxin exposure in long-term E-cigarette and nicotine replacement therapy users: a cross-sectional study’. Annals of Internal Medicine, 166 (6), pp.390-400.
Gale, N., McEwan, M., Eldridge, A.C., Sherwood, N., Bowen, E., McDermott, S., Holmes, E., Hedge, A., Hossack, S., Camacho, O.M. and Errington, G., 2017. ‘A randomised, controlled, two-Centre open-label study in healthy Japanese subjects to evaluate the effect on biomarkers of exposure of switching from a conventional cigarette to a tobacco heating product’. BMC Public Health, 17 (1), p.673.
Institute of Medicine (IOM), ‘2012 Scientific Standards for Studies on Modified Risk Tobacco Products’. The National Academies Press, Washington, DC.
Joanna Hunt
BAT R&D Centre
+44 (0) 2380 588518
Joanna_hunt@bat.com
Tweet @BAT_Sci
www.bat-science.com