The Innovation Platform spoke with the President of the United Kingdom Society for Biomaterials (UKSB), Dr Paul Roach, about the continuing role of the Society, as well as issues such as funding gaps and the clinical need for innovation in biomaterials.
Launched in 2000 with the support of a joint Working Party between the Institute of Materials (IoM) and the Institute of Physics and Engineering in Medicine (IPEM), the United Kingdom Society for Biomaterials (UKSB) is a non-profit organisation working to develop novel biomaterials to tackle current clinical needs for medical devices, prosthetics, and for regenerative medicine. Those with membership have interests in medical materials science, biosensors, biomechanics, biocompatibility, tissue engineering, and many other subjects.
The UKSB community, composed of academics, clinicians, and the biomaterials industry, work together to develop the subject of biomaterials in the UK – a place where biomaterials research and development truly flourishes.
The Innovation Platform spoke with the UKSB’s President, Dr Paul Roach, about the clinical needs and technological pushes of biomaterials, in addition to areas such as funding gaps, the wider context of regenerative medicine, the importance of interdisciplinary approaches, and the continuing role of the United Kingdom Society for Biomaterials.
What would you say are the clinical areas where biomaterials are already playing a key role – or have the potential to do so in the future?
The evolution of biomaterials has been a result of an enhanced knowledge of biology, and perhaps the person who really pioneered this field was Larry Hench who is respected for the development of the new (or next) generation of biomaterials. That is, early modern biomaterials were largely inert and primarily designed to support what was found in the body; but following a drive to better understand biology, these materials were approached with biomimetics in mind, and so became designed to not only support Nature, but also offer a certain bioregenerative capacity, too.
Hench inspired many generations of biomaterials researchers, publishing a formulative review on the advances of biomaterials, with the latest thoughts geared towards the induction of regeneration by cell and gene activation within the biological environment. This, therefore, is indicative of the evolution of biomaterials and, indeed, the direction in which they are headed.
A lot of work has been needed for biomaterials to reach the stage they are at today, and while all biomaterials are designed to try and help the body’s natural processes, some maintain the primary idea of support (such as orthopaedic implants, for instance), while others now include the capacity to regenerate natural material before the biomaterial dissolves away.
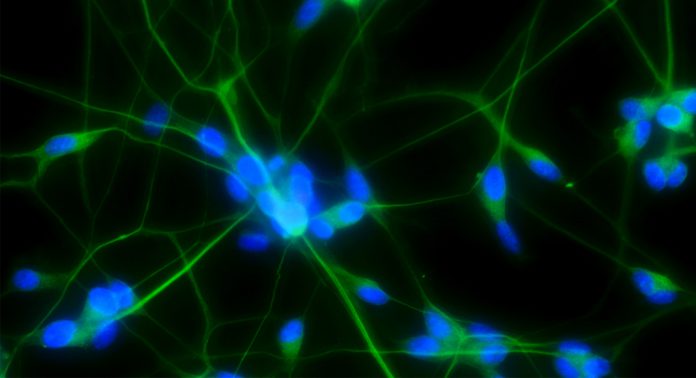
There are some tissues that will naturally regenerate, such as bone (in most instances), and the new generation of biomaterials thus began there. However, over time numerous difficulties and limitations have been encountered in terms of tissues that don’t normally regenerate or don’t regenerate well to give tissue function. To continue with bone as an example: here, there is an architecture in the mineralised form of bone and the cells within it, with the organisation not absolutely reliant on overall tissue function. As such, if a cell is out of place, for instance, when working with a biomaterial, the tissue will still function (though this may not be as optimally as the natural material). On the other hand, in the nervous system or in muscle tissue, for example, the alignment, structure, and connectivity of the cells and their external environment plays a key role in the ability of the tissue to do its job, meaning that everything has to be just right when including a biomaterial for the tissue to function as it should.
The clinical need is thus to create biomaterials which can be used in tissues where organisation is critical. And while there have been some developments in this area in recent years, the major clinical advances have slowed whilst we better understand the fundamental principles of biology and how biological molecules, cells, and developing tissue interact with materials and particularly their surfaces. Without understanding the biology better, we cannot expect to develop better biomaterials; the two go hand-in-hand, as we have seen in the development of biomaterials thus far, and so we need to see these areas investigated to a greater degree before they can be translated into clinical practice.
In addition to clinical need driving the development of new biomaterials, there is also a technology push: the more we understand, the more advanced technologies are created, and this creates something of a virtuous circle. For instance, we have learned a lot about stem cells and their biochemical environments in recent years, and so we are now able to incorporate them into our work by modifying materials or synthetically creating others which include a biochemical cue to infer a direct response to the cells or their surrounding environment.
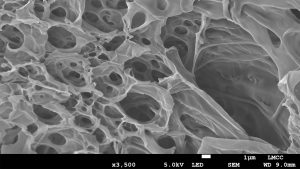
On the technology side, 3D printing is also having an impact. Additive manufacturing, of course, came from the engineering sector. But it has now been translated into medicine (along with many other sectors) so that 3D printed tissues can be made for patients. These tissues have been demonstrated with a span of complexities, the ambition being printing of functional organs.
In a general sense, there is always more to do. For example, while some materials were developed some time ago and are held to be a success, such as those used in a hip transplant, improvements can be made elsewhere. To continue with this example: 30 years ago, a patient receiving a hip transplant would have been in hospital for about six weeks. Now, they can receive the transplant and be sent home in the same day. And this is not necessarily because of developments in the bulk material, but rather in how the materials interact with the host as a result of surface modifications which have made the material better, and there is a lot of work now taking place to improve existing biomaterials via changes in, for example, the nano- or micro texture or, indeed, how that materials is actually put into the body, with some surgical interventions also changing is response to better understanding.
How do biomaterials fit into the wider context of regenerative medicine?
In the same way that the first biomaterials were designed to support tissue, modern biomaterials continue to be designed to this end. However, while the original biomaterials were implanted with a view to the long term (if not permanence), modern biomaterials are increasingly being made to degrade once they have performed their task.
To take bone as the example once more: when a biomaterial is used to plug a bone, as is often the case in treatments for bone cancer, it will be designed to stimulate normal bone growth before naturally degrading to leave the natural material. The bioglass developed by Hench was one of the first to do this.
The plug would be made from a material that will naturally stimulate the regeneration of normal tissue, but because it will necessarily be different to the bone itself, no matter how well made, it can result in a change in properties and so could wear loose or not be properly accepted. The fact that it is able to degrade, however, as well as promote the regeneration of normal tissue growth, means that in the longer term the bone will heal, the biomaterial will no longer be present, and the problem will be overcome. There are nevertheless difficulties which can be experienced here, particularly when it comes to regenerating complex tissues.
Of course, there are instances where a biomaterial needs to be there for the long term and not look to regenerate tissues, like in a hip replacement, for instance. These are biomaterials that aren’t designed to degrade but to provide support for as long as possible, and which go on to be incorporated into the system to support the cells.
© Jordan Roe
Would you agree that there is a need to now look towards new and innovative technologies which are capable of handling multimodal biomaterials and other biological material?
As already mentioned, biomaterials have evolved from a deeper understanding of biology. And as we have developed this knowledge, we have come to understand the complexities of it. For instance, where there was once thought to be just a bone and a muscle, we now know there is indeed a spectrum of biological materials spanning the bone, tendon and muscle characteristics. These changes in tissue properties contribute to the working of the system as a whole. Most biological materials are incredibly complex, and at the moment there is no one technology that can solve all the challenges that we have.
One tool that is widely used to better understand ways of manufacturing biomaterials in the lab is in vitro modelling. And while that is only on a small scale, when we understand these things better, we can go on to translate them, and this is certainly true when it comes to multi-modal biomaterials, particularly with regard to aspects such as changes in stiffness, for instance.
To return to the above example of bone, tendon and muscle: the bone is very hard, the tendon is partly mineralised at the bone end, but can be quite rigid towards the muscle – all of these have a different stiffness. We find a similar thing with the brain: we now understand more about the different types of brain regions and how they are organised in terms of cell types and micro-environments, and in some way we can characterise this by regional stiffness. These differences in stiffness can be inferred by changes in the material that we use. Although this one characteristic may give us some understanding from one perspective, a major drawback is that this is a limited perspective and many more are needed to infer the inner working of complex biology.
The more we explore and the deeper we look, the more links we see. And from this, we can better explore the effects that are inferred when we change the properties of a given biomaterial, or what happens to cells internally when they interact with that material, and so on. And this is certainly of use with regard to stem cells, where a cell might be needed to do something very distinct. For instance, a bone implant will interact with the stem cells in that area, and as pluripotent stem cells can become lots of different types of cell, it could be possible to control that, meaning that they become a cell type of your choosing.
The Biomedical Applications Division of the Institute of Materials Minerals and Mining has highlighted a ‘perceived funding gap between in vitro laboratory research and in vivo validation of results which may limit the translational impact of both university- and industry-based research and development.’ Is this also something that you see as being an issue? Is there enough support for the commercialisation and/or scaling up in the UK in the biomedical space?
In terms of funding, yes there is a gap. It is very difficult to progress to the in vivo use of a biomaterial from in vitro modelling without going through an animal stage. And yet, many animal models don’t work very well for certain tissue types. Thus, there is a reliance on certain tools and technologies that aren’t always fit for purpose, and while we know that this doesn’t work very well, we use it regardless. This is mainly because we don’t currently have a better alternative, or likely the truth is that in some cases we may have some better alternatives but we are used to using the tools that we have, so there is a tendency to continue. Specific funding focussed on the 3Rs is challenging this, not only driving better humanised ‘models’ but also developing new tools and advancing technology and understanding.
In recent years, there has been a lot of cutting edge work in vitro modelling work taking place, but the question of how to translate this from bench-to-bedside has not been resolved, and there is a distinct sense that this is because of a hesitation to use something that isn’t overly familiar. It is here that the gap exists, as funding tends to be available for the fundamental aspects, but the applications are not achieved because the results are not validated due to a lack of a viable alternative to the animal model. We need to develop a way to move fundamental research through to the clinic in a way that is scalable, too.
Manufacturing can also be an issue. The Engineering and Physical Sciences Research Council (EPSRC) has invested in developing a manufacturing strategy, and I was on the Early Career Forum for Manufacturing Research until my tenure recently came to an end. The discussions taking place here were centred on identifying the gaps in manufacturing and how the research council could support tackling the challenges in this hugely multidisciplinary area. It was really inspiring to see that the RCUK are really trying to underpin the excellent research potential within the UK.
The development of biomaterials involves expertise from numerous disciplines. Is enough being done to ensure co-operation and collaboration here – or perhaps to ensure, for instance, clinicians are involved early on?
The biomaterials community is incredibly diverse; it includes those working in areas of biology such as stem cells, as well as others such as neurologists, and everything in between. Many of these people may not have an extensive knowledge of biomaterials. But there are also others who have an in-depth knowledge of (bio)materials but are lacking in knowledge about biology. The two sides are often eager to learn more about what it is their counterparts do. As such, training is now in place to help people to span the two areas.
This is a trend which seems to be picking up pace in recent years. Certainly during my own career I have seen more of this, with people being brought in from fairly disparate disciplines to see how their tools, technologies, and materials can be applied in biomaterials, and that is exciting to see.
The UKSB has an Early Carer Forum within which we work to help those in the early stages of their career feel comfortable in expanding their knowledge base within an interdisciplinary environment. There are also many opportunities to interact with the Society, with funded ‘lab-2-lab’ awards to support work between labs and build strength in the biomaterial’s community.
When I first became involved with UKSB as a first year PhD student, I perceived the meetings to be attended very much by those focused only on biomaterials. But, over the years, I’ve come to understand that this group of people can contribute from vastly different fields of research and interests. I’ve been at meetings speaking with clinicians about their limitations and needs to advance their work, being joined by a physicist or chemist who can address some of these issues using their tool or technology. Many conversations at meetings last well into the evening, with ideas developing and maturing as the discussions ensue. It is always a pleasure to see this, and even more so when these meetings include not only prominent speakers but also those early in their careers. I always encourage my group along; many great ideas come out of these conversations and part of developing the next generation of researchers is to include them in this experience.
Of course, many PhD students or even post docs might feel a little intimidated at first when they find themselves in a room with a world-renowned professor. But that is exactly the environment we are trying to foster. Because when those barriers are broken down, and not only different disciplines but also different levels are put together, results are achieved. Indeed, I enjoy introducing first year PhD students to the UKSB meetings because they begin with a perception of what it will be like, and they may feel quite limited in terms of what input they can have in discussions. But when they come away from the meeting, they are invigorated; they have lots of new ideas and can’t wait to get back to the lab.
The UKSB thus supports interdisciplinary activities in this way, but also by providing a limited amount of funding for those students who have had their interest piqued by the work taking place elsewhere, so that they can visit and learn new things, cross-pollinating labs with knowledge and skills, and importantly strengthening the relationships that underpin future research collaboration.
Along with the UKSB, I am also involved in the Society for Natural Sciences, which is working to bring even more people together to teach them to think outside of the box (which can be a particularly difficult task) across a number of disciplines. In the past, if a student were interested in several subject areas, such as maths, physics, and chemistry when they left school, the previous degree structure meant that they needed to choose just one very early on, or alternatively they needed to study a joint honours degree. But the natural sciences are broader than that. We therefore want to teach people that they can actually work across disciplines, and we therefore bring people with an interest in multiple areas together with the aim of helping them to understand that these subjects can often all be separate elements of one larger whole, and so crossing over into other disciplines should be actively encouraged.
In the UK, there is a significant drive to ensure that people are ambitious in the areas and fields that they want to study, because it is clear that those with ambition help things to develop much faster than those without.
What role will the UKSB continue to play moving forwards?
Fostering interactions with clinicians has always been a difficult thing to achieve due to time constraints and aligning diaries, and so that is certainly going to be a focus area for the future. During the current COVID-19 pandemic we, like so many others, have moved a lot of our activities into the virtual space. This has made it is easier for people to join a meeting, even if only for the parts relevant to them (and so they are more likely to register and take part). This could be a way of including more interactions with clinicians in the future, which is crucial if they are to be involved earlier in projects. The is something the entire community would like to see.
This year, the UKSB decided not to have its usual annual conference, but instead was invited to join with the Centres for Doctoral Training (CDTs) working in this area for a joint virtual conference, and was a resounding success with nearly 300 in attendance. Hosting the event online meant that we were not restricted to the typical two days; rather, we were able to have activities take place over a couple of weeks, and the posters which, in a physical environment, would have been made available for just two days, were available virtually for much longer for people to read and comment on. So perhaps learning to use virtual platforms to our advantage is a benefit to come out of the impacts of the coronavirus, and one that we will continue to look to.
Dr Paul Roach
President
p.roach@lboro.ac.uk
Tweet @Paul_Roach
www.uksb.org.uk
Please note, this article will also appear in the third edition of our new quarterly publication.