Eduardo Pisani, CEO of All.can International, discusses the cancer organisation’s recently-published landmark report entitled Harnessing data for better cancer care.
On 27 May 2021, All.Can published a landmark new report entitled Harnessing data for better cancer care.1 It aims to offer policymakers, care providers, and decision makers a forward-looking view of opportunities for optimising the use of data to improve efficiency in cancer care. It starts by defining data and investigating the current role of data in cancer care and it describes where data have contributed to improving patient outcomes and efficiency across the cancer care pathway, focusing on their role in addressing inefficiencies viewed as important to cancer patients and their caregivers. It then discusses the challenges that remain in optimising the use of data and provides recommendations for policymakers to overcome these challenges.
The report does not attempt to cover all facets of the complex ecosystem of data in healthcare, however. For reasons of feasibility, it focuses on data generated during the provision of routine clinical care and does not include data collected in clinical trials.
The document has been produced by The Health Policy Partnership and Intacare International on behalf of All.Can International. Its creation was led by the All.Can Data Working Group, made up of All.Can International members, and an External Advisory Committee.
Matthew Hickey, CEO of The Health Value Alliance and All.Can International Research and Evidence Working Group Co-Chair, said: “Healthcare systems around the world have not fully harnessed the potential of data to transform cancer care – but we hope to move the needle forward with our report findings and recommendations.”
Types of data
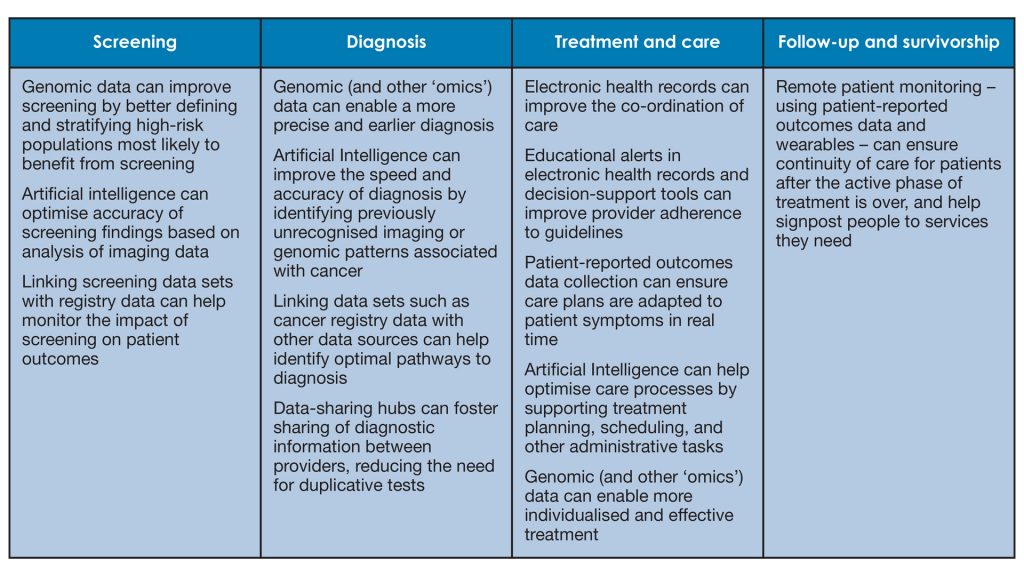
There are numerous types of data that play a role in cancer care, and the report looks in particular at cancer registry data, electronic health and medical records, genomic data, and patient-generated health data. These data have shown the ability to drive quality, innovation, and efficiency in cancer care. This brings tremendous value to individual patients through more accurate diagnosis, personalised treatment, and follow-up care. It also helps healthcare professionals better understand their patients’ needs and adapt care accordingly. At a system level, large-scale data collection can lead to improvements in care and provide insights into which aspects of care offer the greatest impact on patients and health system efficiency.
The report also includes case studies that provide concrete examples of how data have transformed cancer care, which can be emulated elsewhere. “Having good data is everything,” said Christobel Saunders, Professor of Surgical Oncology at the University of Western Australia and All.Can International Research and Evidence Working Group Co-Chair. “We need good data on individual patients, on how our teams and hospitals are functioning, and we must be able to compare these data to ensure we can correct any unwanted variations in patient outcomes.”
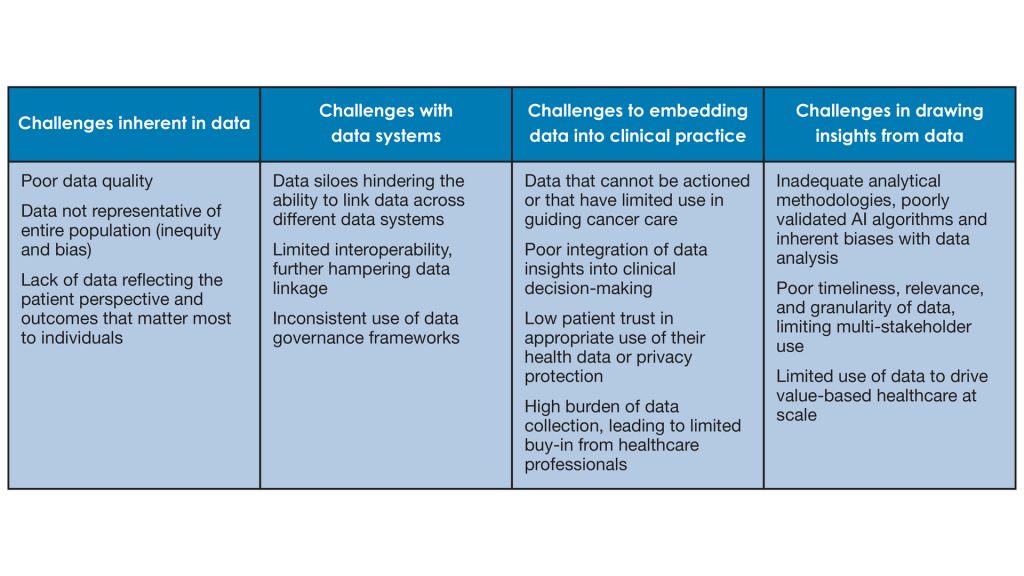
She added: “Currently, data siloes, a lack of interoperability, unclear actionability of existing data, complex data governance, and limited ability to re-use data for other purposes are all on-going challenges in many countries, and we often fall short in our ability to analyse and extract meaningful insights from the data available to guide decision-making.”
Overcoming these challenges is integral to ensuring the sustainability of health systems and delivering better care for patients.
These goals are especially pertinent in the context of the COVID-19 pandemic and health system recovery. Dr Vivek Muthu, Managing Director of Marivek Healthcare Consulting and All.Can Member, said: “We need to think of data as an investment, but also as an innovation. Having the correct data systems in place, to be able to harness their value, is as important to the future of cancer care as new medicines and other advances.”
The power of data to transform cancer care
Cancer care is advancing at a speed never before seen, and data are at the core of many of these advances. Data are the foundation of a learning healthcare system – enabling improvements in both efficiency and quality of cancer care across the entire care pathway.
The amount of data we now have at our disposal is considerable – as well as the insights we can draw from it. Mobile applications and smart devices now enable the collection of health data in a person’s daily life outside of clinical settings, allowing for remote monitoring and identifying critical health events sooner.
Different sources of data can be combined and analysed thanks to machine learning and processing speeds never seen before, as well as Artificial Intelligence (AI).
The result is that we are now able to solve some of the most complex challenges in healthcare at a scale and speed that were previously impossible.
We are still far from fully harnessing the potential of data to transform cancer care
Despite their enormous promise, several hurdles hinder our ability to fully harness data to their full potential. Many of the advances mentioned above are still at early stages of implementation, and the notion of ‘data rich, information poor’ rings true in cancer care. Persisting challenges remain in the quality of data, the systems used to collect them, integrating data into clinical care, and using data to draw meaningful insights to drive change.
Some of the most pressing challenges are summarised below:
Data are not always representative of entire populations (inequity and bias)
Inequities in data can take several forms, introducing biases in the availability of data about certain populations defined by race, ethnicity, or socioeconomic status, as well as varying amounts of data available for different types of cancer. Current data equity challenges mean that not all people benefit equally from data innovations in cancer care – with, traditionally, data collection favouring Western and Caucasian populations. Without data specific to given populations, it is difficult to know the impact of cancer or health interventions on those groups. Data can also be biased towards different types of cancer. For example, most cancer registries do not collect data on cancer recurrence, therefore information is particularly scarce on people with metastatic cancers. Similarly, lack of available data on some rare cancers like brain and CNS tumours has traditionally resulted in limited research opportunities or innovations for these conditions, leading to fewer treatment options for patients. Policymakers can help create greater equity in data collection by:
- Demanding greater equity in cancer research and care by ensuring appropriate representation of people of different races and ethnicities, sex, and cancer types in cancer data sets;
- Holding institutions accountable for providing equitable cancer care by capturing performance on key quality indicators according to patients’ race, ethnicity, sex, and socioeconomic status; and
- Ensuring proportionate allocation of funds towards specialist cancer registries to collect data on different populations of cancer patients for whom data are less available.
We lack data reflecting the patient perspective and outcomes that matter most to them
Patient-generated health data, such as patient-reported outcomes measures and patient-reported experience measures, are vital to our understanding of the patient’s perspective on quality and impact of their care. Yet these data are still not always collected as part of routine care. Even when they are collected, patient-reported data are not always used to guide patient care. As a result, we miss opportunities to make each person’s care more patient-centred, and to gain a complete picture of how healthcare systems are performing from the point of view of the people they are designed to serve.
To create more patient-centred data collection, policymakers should focus on:
- Encouraging systematic and standardised collection of patient-generated health data, such as measures of patient-reported outcomes and patient-reported experiences, in key national health data sets; and
- Including these data in regular monitoring and performance evaluations of cancer care to guide improvements most relevant to patients.
Patients may not always trust that their data are being used appropriately and may have concerns over data privacy
It is important to never lose sight of the fact that people whose data are being collected have a right to know how their data are being used. Public opinion research shows a willingness from both patients and the general public to share personal health data for research purposes, but on the condition that it is done securely, and that data are accessible only by authorised parties.
Each person should know the goals of research involving their data, and how they can opt out. Fostering transparency in data use across cancer care helps to build public trust in data collection efforts. Continued conversations, education, and an open dialogue with patients and the general public are important to ensure their data privacy and confidentiality concerns are being addressed.
To build patient trust and protect patient interests in data sharing, policymakers should focus on:
- Creating public awareness and education campaigns to convey the power of meaningful data to better manage cancer care;
- Engaging with patients and patient representatives to discuss how data are being used, and address misconceptions around the nefarious use of health data; and
- Continuously adapt legislation and tools to give citizens appropriate control over their own health data, so they may act as their own data ‘gatekeepers’.
The way forward
The potential of data to improve cancer care is considerable – but it will only be achieved if we overcome existing challenges to their collection and use. Having the correct data systems in place and being able to harness their value is as important to the future of cancer care as new medicines and other advances. It is also integral to ensuring the sustainability of health systems and delivering better care for patients.
The report hopes to offer solutions and a useful starting point to drive change and shift the needle in optimising the use of data in cancer for the benefit of all cancer patients, leaving nobody behind.
Quality cancer care relies on us taking a data-driven approach to decision-making – for each individual patient, for the population as a whole, and across all steps in the care pathway. This can only happen if we invest in making sure the data we collect are of the highest quality and relevance. We need to make appropriate linkages between existing data systems and use the right tools to draw insights from them. Finally, we need to build data into continuous improvement measures at an individual, organisational, and national level.
As part of the digitisation agenda, policymakers must implement lasting changes across systems of care and policy frameworks to enable data to achieve their full potential for the benefit of all people with cancer. Commitment is needed to embed optimal use of data across all facets of cancer care, in all settings, for all people living with and beyond cancer.
About All.Can International
All.Can International is a multi-stakeholder, not-for-profit organisation (ASBL) registered in Belgium that aims to identify ways in which resources in cancer care can be used more efficiently, with the goal of achieving better patient outcomes.
In alignment with its statutes and bylaws, all activities and outputs of All.Can represent consensus of members who have full editorial control. For more information about All.Can, its full membership and governance, visit: www.all-can.org
Its work is made possible with financial support from Bristol Myers Squibb (main sponsor), Roche (major sponsor), MSD and Johnson & Johnson (sponsors), Baxter and Illumina (contributors), with additional non-financial (in kind) support from Helpsy, The Health Value Alliance, and Goings-On. In addition, this report received financial support from Novartis.
Further information
All.Can Secretariat Contact: secretariat@all-can.org
All.Can Data Report Contact:
Shannon Boldon, shannon.boldon@hpolicy.com
References
- The full report is publicly available on the All.Can website (www.all-can.org)
Eduardo Pisani
Chief Executive Officer
All.Can International
+32 2 761 66 73
secretariat@all-can.org
Tweet @AllCanGroup
www.all-can.org
Please note, this article will also appear in the seventh edition of our quarterly publication.