The InterOrtho Research Group at Aalborg University Hospital in Denmark aims to develop an entirely new research area of improved patient care through advanced sensor technologies.
Patient care is radically changing towards hospital at home solutions. In the event of bone injury or planned surgery, patients will demand fast recovery at home and early return to everyday life. The InterOrtho Research Group at Aalborg University Hospital in Denmark is developing a novel research area of improved patient care via advanced sensor technologies.
The challenge with point-by-point data
After surgery, patients are typically followed for several weeks where they are scheduled at the outpatient clinic for one or more check-ups. At the hospital, X-rays are taken, or physical examinations are performed to see if the expected progress has taken place.
Current practice is defined by hospital logistics. Patients often are discharged immediately after surgery as increasingly more surgeries are performed on an outpatient basis. At the same time, the number of outpatient check-ups is reduced, which means that the healing and progress after an operation is only monitored point-by-point.
At the check-ups, clinicians can ascertain whether there is the desired progression in the healing process or whether the development requires intervention. Unfortunately, spot checks also mean that clinicians can only see complications such as lack of healing or infection when the complication has already occurred, rather than beforehand.
Today, the planning of outpatient check-ups is based on historic data from large patient populations, which reflects the expected development of the type of surgery in question. These are time-shifted average data that do not consider the individual patient’s physiology or conditions surrounding the operation. Thus, it is not the patient’s own data that defines how the follow-up should be organised and when a possible intervention should be initiated.
Sensors and software to ensure continuous monitoring
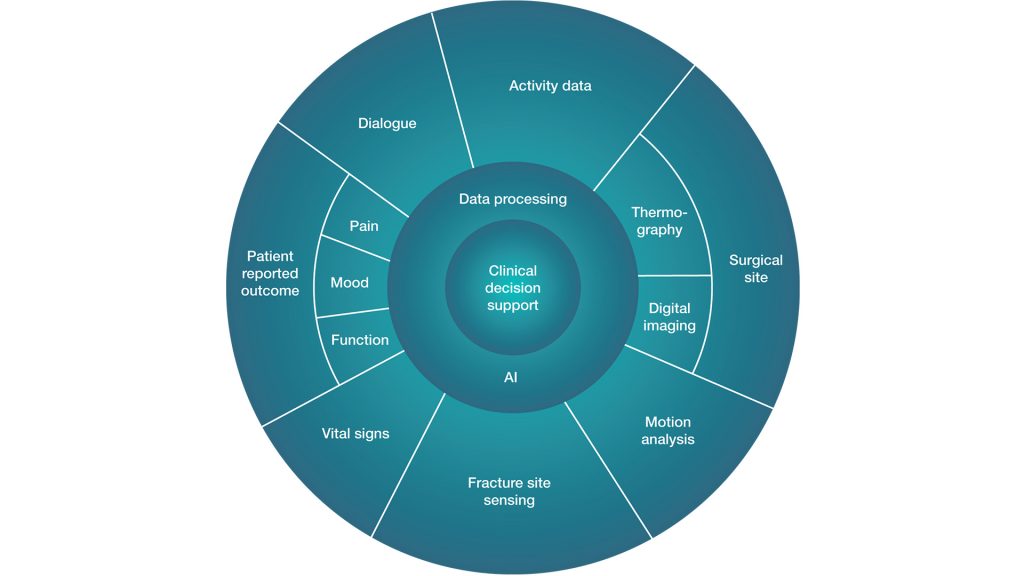
The orthopaedic surgery research group InterOrtho, at Aalborg University Hospital, develops and validates modern technology based on sensors that can continuously collect data about patients while they are at home, independent of the planned checks at the hospital. By doing this, patients’ treatment can be individualised and complications may be detected at an earlier stage. Additionally, large amounts of data can be generated for prediction models that can provide individualised estimates for future patients on how they will perform after surgery (Fig. 1).
Such an ambition presupposes technology development on several fronts. One is to develop suitable sensors – Internet of Things (IoT) solutions that can be implemented in clinical practice, either in the form of implantable microsensors, wearable sensors, or via software implementations on the patient’s smartphone.
Inertial sensors have the potential to take on a more prominent role for continuous gait and motion analysis after orthopaedic surgeries in real-world conditions and during daily activities. There are already several technologies on the market today that can monitor, for example, physical activity. These are primarily developed for leisure exercisers (running, walking, strength training, etc.), and it is therefore not given that the same technologies are able to provide valid data in patients who have had surgery on the hip or knee. An essential part of our research is therefore to validate the technologies among patients.
The more data sources and the more data points that can be generated, the better basis the clinician has for making individually tailored decisions about treatment and intervention. But to translate the large amount of information into, for example, preventive interventions, the development of deep learning models is needed.
This work of developing and refining the clinical applicability of these technologies takes place in close collaboration with leading international experts in biomechanics and musculoskeletal modelling from Aalborg University, who, among other things, have special expertise in processing raw data from existing sensor technologies, and translating these into clinically applicable algorithms.
Current projects
In the InterOrtho Research group we have defined a number of projects as part of the Clinical Intelligence project with the ultimate goal of developing a deep learning algorithm for the postoperative monitoring of patients at home. In the following some of these will be presented.
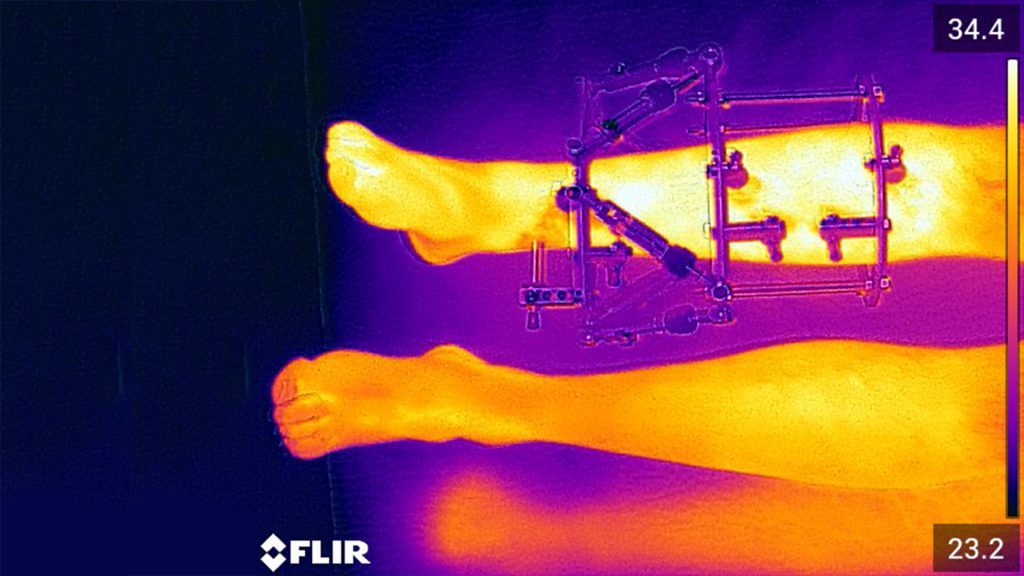
Home-based monitoring with thermography for detection of postoperative infection
Thermography may be useful in monitoring surgical sites for infection but has not yet been implemented in telemedicine. As thermography is presently being integrated into mobile phones or can be used as an add-on to standard phones, this technology is opening new possibilities for home-nurses, relatives, or patients to perform infection surveillance.
The aim of the thermography studies is to examine whether thermography can be used as a homebased postoperative surveillance in orthopaedic patients to detect or predict wound infection. We seek to define a point of care for infection.
Infection has been estimated to account for 0.5% of hospital budgets in Denmark and represents a significant morbidity to the patient. Today, patients are discharged earlier from hospitals, shifting the postoperative surveillance to the patient’s home. The care is thus transferred from the highly specialised hospital to surveillance by municipality home-nurses and general practitioners. During this shift, both information and knowledge of postoperative care is often lost, leaving the patient with uncertainty. This uncertainty is enhanced by a lack of agreement on the definition of infection and little evidence of systematic measurement and monitoring of wounds after discharge. Therefore, point of care technologies are important.
The setup is multidisciplinary, international cross-sectional and longitudinal studies. The thermography studies will focus on orthopaedic patients with external frames (Fig. 2). These patients are at considerable risk of infection during a treatment period of several months, and an infection in the worst-case scenario can be limb threatening. The experience and knowledge we will obtain from this project can be used in general to improve care for patients after surgery in the future.
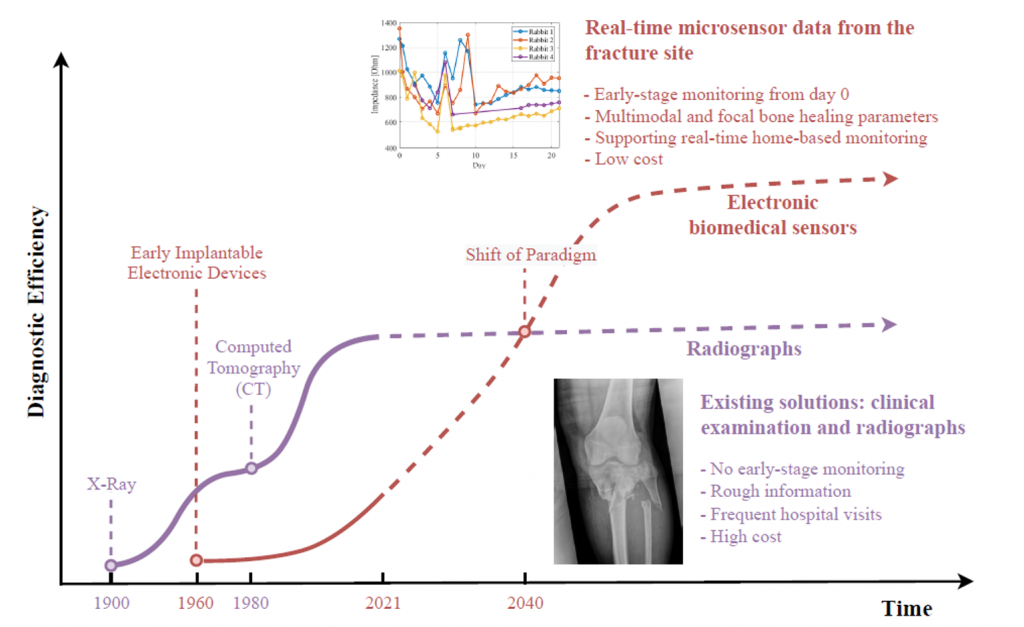
Implantable sensors for monitoring bone healing
In a current experiment we are investigating whether wireless sensors that are implanted on each side of a bone fracture can pave the way for a replacing of X-rays when it comes to observing whether bone healing is progressing as planned (Fig. 3 ). The electrodes send a current through the broken piece of bone and by measuring the electrical resistance that occurs between the electrodes, deviations from normal bone healing might be detected. Preclinical pilot-tests have shown that the technology correlates with bone healing.
A current challenge stems from the fact that spot checks with X-rays are unable to predict which fractures will not unite, and the diagnosis of non-healing can only be made after six months. The result may be chronic pain or loss of function. With continuous monitoring, it will be possible to make adjustments that can ensure optimal adhesion of the fracture.
Improved monitoring of bone healing will also have the advantage that, in the future, it will be possible to offer more individually tailored rehabilitation, meaning that the patient’s training and physical activity can be co-ordinated with the progression of the bone healing.
Motion analysis
One of the most important daily activities is walking. Ambulation plays a crucial role in the recovery of patients after orthopaedic surgeries and those patients are encouraged to start walking after the surgeries to accelerate the process of recovery. We believe that the changes in quantity and quality of the gait during the post-op period represent the characteristics of the recovery process. Analysing the gait attributes can be used to assess recovery. However, the complexity of gold standard methods for gait analysis has limited their application during the post-op recovery period. A possible solution might be found in wearable sensors or motion capture analysis applying algorithms originally developed for the animation film industry.
Employing deep learning models for the investigation of the data derived from these sensors may facilitate patients’ home monitoring in the future. Currently, studies in patients after knee arthroplasty are employed. In the future, telemedicine motion caption analysis via mobile phones is predicted to have a huge potential in orthopaedic rehabilitation as motion analysis may be captured and analysed in real time by the mobile phone. Studies are currently being drafted to validate this technique.
The Dialogue Project
A key element in our ambitions to create an Artificial Intelligence algorithm for optimising patient flow is developing a communication platform that places the patient at the centre of communication between all parties involved in the process. That can be relatives, general practitioners, physiotherapists, home nurses, social workers, and medical staff at the hospital.
Through an application on the patient’s smartphone, patients and health professionals across Aalborg University Hospital and Aalborg Municipality will be able to communicate in simple text messages. We want to explore text messaging with the patient as a simple communication tool in rehabilitation after orthopaedic surgery.
Current communication pathways are slow, inefficient, and cause frustration among both patients and health professionals. In the worst cases it compromises patient safety, when important knowledge is not shared in a timely fashion, or treatment regimens are not understood. After discharge, surgery patients may have questions or concerns leading them to call the general practitioner, home care nurse, or the hospital for answers. Often, they reach a secretary, rather than the specialised healthcare team at the hospital. Organisational barriers between hospital and municipality challenge communication, leading to patients experiencing a lack of coherence in the healthcare system.
By introducing a text messaging app, where patients, hospital staff, and staff from the municipality can communicate, we believe it will be easier for the patient to get clarification on questions, and the co-ordination and knowledge sharing between the hospital and the municipality will be more flexible and individualised. At the same time, the patient is placed at the centre of the dialogue, which we hope can help empower patients and relatives, and maybe even health professionals across sectors. Future research will look into if these dialogue data can be used as data points in prediction models.
Diversity in skills and knowledge is needed
We strive for high diversity in our group to provide the needed synergy and expertise to make high-impact innovative research. Our philosophy is that the highest level of domain knowledge is needed both from the clinicians and the engineers. All solutions are patient centred, which dictates a close and day-by-day collaboration between clinicians, patient representatives, and engineers. Our innovation is based on research to provide data for evidence-based decisions when adapting new technology into clinical practice.
What we do today creates a better tomorrow
Implantable sensors that use electricity to measure whether a fracture heals as it should and the use of a mobile phone’s camera to predict an upcoming infection may sound like science fiction. Many of the technologies we work with are still at a very early prototype stage and may not be ready for clinical application until many years from now. Nevertheless, it is important that the technologies are developed and adapted based on clinical research.
Therefore, it is our hope that our work can inspire even closer collaboration between clinicians and engineers, as we believe that only through joint efforts can we create innovative solutions that can meet the health challenges of the future.
If you would like to know more about our work at the InterOrtho Research Group at Aalborg University Hospital or would like to collaborate with us, please do not hesitate to contact us.
Initiators of Interdisciplinary Orthopaedics
Clinical Professor Ole Rahbek, MD, PhD is head of Children’s Orthopaedics at Aalborg University Hospital, Denmark. His main research area has been children’s orthopaedics and how to improve the surgical care of children with disabilities. Optimal surgical care is to prevent surgery if possible and, in the case of surgery, minimising the time the child and family spend in hospital, by the use of digital health solutions.
Clinical Professor Søren Kold, MD PhD is head of Limb Reconstruction at Aalborg University Hospital, Denmark and is a well renowned international expert in treating highly complex fractures and complications. He has previously introduced new technology from preclinical in vitro and in vivo research into orthopaedic randomised clinical trials.
Associated Professor Ming Shen is leading the AI RF Sensors group at the Department of Electronic Systems, Aalborg University. His current research interests mainly include digital healthcare technologies, especially wireless microsensors and Artificial Intelligence (AI) in orthopaedics.
Research collaborators for clinical intelligence
To create digital solutions for the patient, a broad coalition is needed to cover all aspects of patient care with the aim of implementation after validation.
Aalborg University:
- Department of Materials and Production; • Department of Health Science and Technology; • Department of Electronic Systems; and • Department of Engineering and Science Faculty.
Aalborg University Hospital:
- Institute of Biomedical Research;
- Unit of Clinical Biostatistics; and
- Health IT.
Aalborg Municipality:
- Quality and Innovation.
National partners:
- Danish Paediatric Orthopaedic Research; • Orthopaedic Research Laboratory, University of Southern Denmark; • Alexandra Institute and Institute of Computer Science; • Institute of Public Health, Aarhus University; and • Danish Technological Institute.
International:
- Texas Scottish Rite Hospital for Children, Dallas, Texas, USA; and • Nationwide Children’s Hospital, Columbus, Ohio, USA.
Private:
- Synoste;
- Visma A/S;
- Trifork A/S;
- BioX;
- AnyBody Technology A/S;
- Data For Good Foundation.
Please note, this article will also appear in the eighth edition of our quarterly publication.