Dr Makoto Ikeya discusses his work at the Center for iPS Cell Research and Application (CiRA) at Kyoto University and explains how induced pluripotent stem cells (iPS) technologies stand to impact on the future of human health.
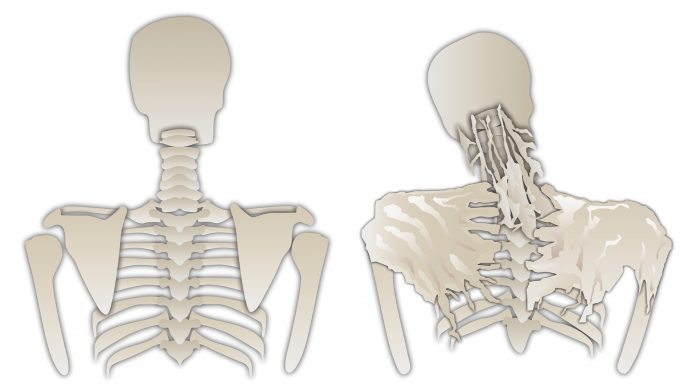
BY using iPS cell technology, Dr Makoto Ikeya’s lab at the Center for iPS Cell Research and Application (CiRA) at Kyoto University, Japan, is currently focusing on incurable diseases that occur in mesenchymal tissues such as bone and cartilage, and for which effective treatment has not yet been developed.
Induced pluripotent stem cells (IPSCs) can be applied to address the accidental loss of cells or the impairment of cell functions in the human body. Cell transplantation can be applicable for the lost cells and functional impairment could be restored through the investigation of the molecular mechanisms of disease occurrence.
iPS cells can be applied in both cases. Regarding the former, the development of an efficient induction methods into specific cell types or tissues enables the use of these cells as a source of transplantation therapy, and for the latter, in-depth analyses by using disease-specific iPS cells will lead drug innovation.
In Ikeya’s laboratory, the team are placing a focus on employing both approaches to tackle refractory osteochondropathies. They are establishing a differentiation methods from human iPS cells to mesenchymal cells, which is necessary in the process of disease recapitulation and for transplantation. Their aim is to develop a new remedy for incurable diseases through this series of approaches.
Speaking to Innovation News Network, Ikeya discussed his work and explained how iPS cell technologies stand to impact the future of human health.
How important is the investigation of the roll of pluripotent stem cells when it comes to research into (currently) incurable diseases?
The generation of iPSCs represents a unique technology which is useful for basic research as well as clinical applications. This was developed in 2006 by Shinya Yamanaka, who is now the President of the Center for iPS cell research and application (CiRA) at Kyoto University. iPSCs are similar to embryonic stem cells (ESCs) in terms of their multiple differentiation property and unlimited proliferation ability. But since iPSCs are made from somatic cells and there is no need to destruct human embryos, iPSCs are somewhat ethically advantageous. Moreover, if iPSCs are generated from the somatic cells of patients suffering from a disease, then the patient-specific iPSCs can be used for disease modelling and drug discovery because the occurrence of the disease can be recapitulated in vitro.
How are you using disease-specific iPS cells to tackle refractory osteochondropathies? What are the biggest challenges then to progressing to drug discovery/development?
To maximise the power of iPSC technology for disease modelling and drug discovery, there are two requisite technologies: robust differentiation protocols to desired lineage cells, and ideal control iPSCs.
iPSCs are in a pluripotent state and it is assumed that they are equivalent to the epiblast stage in embryos. This means that, in order to correctly model disease phenotypes, it is necessary to induce target cells from iPSCs. At our lab, in collaboration with Professor Toguchida’s laboratory and Sumitomo Dainippon Pharma, we have been focusing on an intractable rare osteochondral disease, fibrodysplasia ossificans progresssiva (FOP), which is characterised by ectopic endochodral ossification formed in soft tissues such as skeletal muscle and tendon/ligament. Although it is still under discussion, a cell-of-origin of ectopic bone/cartilage is mesenchymal stem/stromal cells (MSCs). We have developed a simple and robust protocol to induce MSCs from human iPSCs and have used them for our research.
A second important challenge is how to prepare ideal control cells. Since patient-specific iPSCs are derived from individual patients, the genetic backgrounds are varied. Therefore, observed differences between patient-derived iPSCs and healthy wild-type control iPSCs may reflect the difference between original individuals. Moreover, iPSCs have clonal variations, resulting in different phenotype strengths even amongst clones generated from the same patient. However, genome editing technologies enable us to generate mutation-corrected iPSCs from patient-specific iPSC clones. Based on our experiments, experimental variations are minimised when we use mutation-corrected iPSC-derived cells.
In summary, robust induction protocols and mutation-corrected control iPSCs enable us to minimise experimental error and establish a highly-sensitive detection system for disease modelling.
By using FOP iPSCs and the above two technologies, we have succeeded in recapitulating the FOP phenotype; we have screened small chemical compounds and identified one chemical, Rapamycin, which has the potential to prevent the progression of FOP. Based on this achievement, our collaborator Professor Junya Toguchida started clinical trials in 2017 in Kyoto University Hospital. This is the first trial to use a chemical identified through an iPSC-based high-throughput screening system.
How important are mesenchymal stems cells (MSC), and in particular iPSC-derived MSCs (iMSC), to you work? Where are you in overcoming relevant challenges before the clinical application of iMSCs?
In our case, iMSCs were used for the in vitro modelling and drug screening of FOP. This, of course, is one of the most promising way to use iPSCs. There is, however, another important way of using iMSCs, namely cell-based therapy that complement lost cells/tissues/organs in patients.
Primary MSCs can be isolated from several adult tissues such as bone marrow, adipose tissue, and dental pulp. They can also be isolated from perinatal stage tissues such as umbilical cord blood, decidua, Wharton’s jelly, and placenta. They are already applied in clinical uses such as graft versus host disease (GvHD), stroke, multiple sclerosis, and spinal cord injury. There is a lot of knowledge about the safety of MSC transplantation because, historically, in hematopoietic stem cell transplantation MSCs were co-transplanted to provide a supportive environment, and no hazardous events were observed.
In the case of iMSCs, there are advantages and disadvantages compared with primary MSCs. As iPSCs can proliferate, they can theoretically supply iMSCs in unlimited cell numbers, whereas the proliferation ability of primary MSCs are highly dependent on individuals. Moreover, the quality control of iMSCs is easier than that of primary MSCs because the quality can be stabilised by well-established induction protocols.
If HLA-matched iPSCs are used as the source of iMSCs, the problem of immuno-rejection can be overcome, whilst the autologous transplantation of primary MSCs is theoretically the best. The most ambitious prediction is that there are diseases curable only by iMSCs administration. The population of primary MSCs is heterogeneous, while iMSCs could be homogeneous. As such, it is likely that such an application will be discovered. However, we need more basic research to move towards that.
How do you feel that iPSC and iMSC production protocols could be optimised? And how can it be ensured that any ethical issues are addressed?
The protocol optimisation of iMSC production is mainly judged by the in vitro proliferation and differentiation properties. We use commercially-available xeno-free MSC medium for iMSC induction because of the possible future clinical applications. However, in many cases iMSCs would not be able to survive in a commercially-available xeno-free MSC medium. We do not know the exact reason for this, but it may be due to the fact that iMSCs require nutrition. As such, we first screen the medium by the proliferation ability of iMSCs, and as a second criteria we screen the medium along with the differentiation properties. In the minimum criteria of MSCs, they should differentiate into tri-lineages, like osteocyte, chondrocyte and adipocyte, which we also check.
When it comes to the safety of the transplantation into humans, clinical trials of iPSC-derived cell transplantations have already started. In 2014, retinal pigment epithelium induced from iPSCs were transplanted into an age-related macular degeneration patient’s eye. In 2018, iPSC-derived dopaminergic neurons were transplanted into Perinson’s disease patients. In addition, in 2018, Cynata therapeutics, an Australian bio company, announced that Phase I clinical trial using their iMSCs to acute steroid-resistant GvHD was successfully completed. We should carefully monitor how this progresses since iPSC-based therapy is just beginning and it is difficult to predict all of the future issues.
Where will your future research priorities lie?
I am a basic scientist with a strong interest on clinical applications. With that in mind, I am now engaging in the T-CiRA programme, which is a joint programme between the Takeda pharmaceutical company and CiRA. I have a team separate from that in Kyoto, where we focus on neural crest cells and their derivatives for use in future clinical applications. The team members are enthusiastic about therapeutic application of neural crest cell technology and this project has also been progressed steadily.
Acknowledgement: I want to thank to all the people who contributed to our projects, especially Dr Kyosuke Hino from Sumitomo Dainippon Pharma for finding Rapamycin.
Dr Makoto Ikeya
Center for iPS Cell Research and Application (CiRA)
Kyoto University
+81 75 366 7054
mikeya@cira.kyoto-u.ac.jp
www.cira.kyoto-u.ac.jp/e/research/ikeya_summary.html