A new study from the University of Wisconsin-Madison suggests that chemotherapy drugs may not reach their full potential.
This could be because researchers and doctors have long misunderstood how some of the most common chemotherapy drugs actually ward off tumours.
For decades, researchers have believed that a class of drugs called microtubule poisons treat cancerous tumours by halting mitosis, or the division of cells.
However, the researchers found that in patients, microtubule poisons don’t actually stop cancer cells from dividing. Instead, these drugs alter mitosis — sometimes enough to cause new cancer cells to die and the disease to regress.
The research, ‘Diverse microtubule-targeted anticancer agents kill cells by inducing chromosome missegregation on multipolar spindles,’ was published in PLOS Biology.
How do chemotherapy drugs affect mitosis?
Cancers grow and spread because cancerous cells divide and multiply indefinitely, unlike normal cells, which are limited in the number of times they can split into new cells.
The study’s findings are based on a specific chemotherapy drug called paclitaxel. Sometimes prescribed under the name Taxol, paclitaxel treats common malignancies, including those originating in the ovaries and lungs.
Beth Weaver, who led the research, explained: “For decades, we all thought that the way paclitaxel works in patient tumours is by arresting them in mitosis.
“In cells in a dish, labs worldwide have shown this. The problem was we were all using it at concentrations higher than those that actually get into the tumour.”
Weaver and her colleagues wanted to know if other chemotherapy drugs work the same way as paclitaxel – not by stopping mitosis, but by messing it up.
The question has significant implications for scientists searching for new chemotherapy drugs. This is because drug discovery efforts often hinge on identifying, reproducing, and improving upon the mechanisms believed to be responsible for a compound’s therapeutic effect.
While microtubule poisons are no panacea, they are effective for many patients, and researchers have long sought to develop other therapies that mimic what they believe the drugs do. These efforts are ongoing even though past attempts to identify new compounds that treat cancer by stopping cell division have reached frustrating dead ends.
“There’s still a lot of the scientific community that’s investigating mitotic arrest as a mechanism to kill tumours. We wanted to know if this matters for patients,” said Weaver.
How the drugs affect tumour cells in patients
The team studied tumour samples taken from breast cancer patients who received standard anti-microtubule chemotherapy at the UW Carbone Cancer Center.
They measured how much of the chemotherapy drugs made it into the tumours and studied how the tumour cells responded.
They found that while the cells continued to divide after exposure to the drug, they did so abnormally. This abnormal division can lead to tumour cell death.
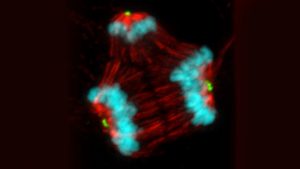
Normally, a cell’s chromosomes are duplicated before the two identical sets migrate to opposite ends of the cell mitosis in a process called chromosomal segregation. One set of chromosomes is sorted into each of two new cells.
This migration occurs because the chromosomes are attached to a cellular machine known as the mitotic spindle. Spindles are made from cellular building blocks called microtubules. Normal spindles have two ends, known as spindle poles.
The hunt for new drug discoveries
The team found that paclitaxel and other microtubule poisons cause abnormalities that lead cells to form three, four or sometimes five poles during mitosis, even as they continue to make just one copy of chromosomes.
These poles then attract the two complete sets of chromosomes in more than two directions, scrambling the genome.
Weaver explained: “After mitosis, you have daughter cells that are no longer genetically identical and have lost chromosomes.
“We calculated that if a cell loses at least 20% of its DNA content, it is very likely going to die.”
These findings reveal the likely reason why microtubule poisons are effective as chemotherapy drugs for many patients. Importantly, they also help explain why attempts to find new drugs based solely on stopping mitosis have been so disappointing.
Weaver concluded: “We’ve been barking up the wrong tree. We need to refocus our efforts on screwing up mitosis and on making chromosomal segregation worse.”