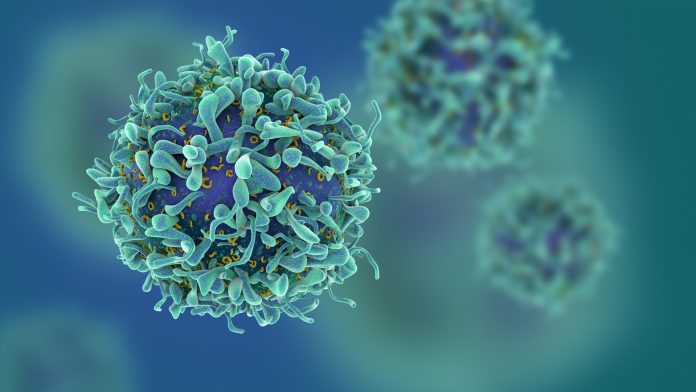
Researchers have developed a new method of quickly generating T-cells, which are used in cancer immunotherapy to destroy tumour cells.
In the September issue of Cancer Research, Hannah Knochelmann, a student in the Medical Scientist Training Program at the Medical University of South Carolina (MUSC), USA, and researcher in Chrystal Paulos’ laboratory teamed up with investigators at three different cancer research centres – MUSC Hollings Cancer Center, Emory Winship, and The James at Ohio State University – to report a new method of generating T-cells faster for patients in the near future.
This team cut down the time needed to manufacture T-cells from several months to less than one week by using a remarkably potent CD4 T-cell subset, called Th17 cells. Knochelmann explained: “In fact, very few Th17 cells were needed to eradicate multiple different types of tumours effectively. This new milestone could widen inclusion criteria to promote access to T-cell therapy for more patients with metastatic disease.”
Adoptive T-cell transfer therapy often uses billions of CD8 T-cells, which have cytotoxic properties that allow them to kill cancerous cells. However, it takes weeks of growth in cell culture to grow enough CD8 T-cells to be used in a single treatment. Paulos, the director of Translational Research for Cutaneous Malignancies at Emory University, said: “What is most remarkable about this finding is that we can build on this platform to bring T-cells to patients all over the world.”
In this new method of generating T-cells, the team grew Th17 cells in cell culture for only four days before being infused into the host. Any shorter or any longer in culture reduced the efficacy of the treatment. While the team could generate more Th17 cells over several weeks, more cells were equally or less effective compared with fewer Th17 cells expanded only four days.
Knochelmann and the team sought to develop a therapy that was long-lived while understanding factors that can prevent relapse. They found that day-four Th17 cell therapy provides a long-lasting response. Interestingly, IL-6 was a key cytokine in fuelling these T-cells to prevent relapse after treatment. This cytokine destabilised the regulatory T-cells which empowered the Th17 cells to kill cancer cells.
Paulos said: “This treatment has the potential to be very versatile. If the tumour can be targeted, meaning that a unique identifier for the tumour is known, this treatment can be effective. Thus, this therapy can be used to treat patients with either liquid or solid tumours.”