A new study by Uppsala University, Sweden, has shown the differences in how Rituximab, a monoclonal antibody drug, interacts with the blood of healthy individuals compared to patients with chronic lymphocytic leukaemia.
This new analysis method could result in important breakthroughs in immunotherapy research and treatment. Innovation in immunotherapy has helped to increase survival rates among cancer patients, but more effective tools are still needed to predict how these drugs will affect an individual’s immune system.
Uppsala University researchers compared what happens when Rituximab monoclonal antibodies interact with the blood of both healthy individuals and of patients with lymphocytic leukaemia. The results showed that the immunological activation markers differ between the groups – an observation that could enable new scientific breakthroughs.
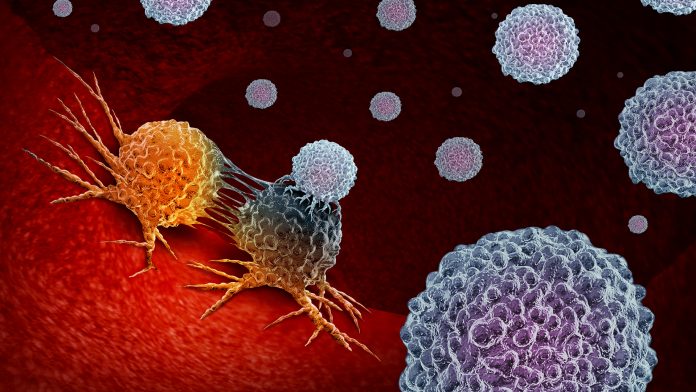
Sara Mangsbo of the Department of Pharmaceutical Biosciences said: “Rituximab is used to treat a range of diseases in which B cells are malignant or growing out of control. The monoclonal antibody binds to the CD20 protein expressed on the B cell and draws natural killer (NK) cells, a part of the immune system, to the site which then help to kill the B cell. The action of Rituximab is specific with few side effects, but when it binds to B cells it can also activate proteins in our blood that signal danger. This can cause Cytokine Release Syndrome (CSR) – normally with mild symptoms in the form of nausea and fever, but it can also become life-threatening.”
Using a human whole blood model
The researchers used a complete human whole blood model to analyse the immune response, and the efficacy and toxicity of treatment with Rituximab. In healthy individuals, only a reduction in the number of B cells was observed. In patients with chronic lymphocytic leukaemia, however, a variable reduction in the number of B cells as well as CRS were observed – except in one patient who had no NK cells. The results increase our understanding of what happens when Rituximab encounters blood from patients with chronic lymphocytic leukeamia.
The use of a human whole blood model in this analysis allow the researchers to consider all the immune cells circulating in the blood, as well as the proteins and metabolites present in the blood serum. The method thus adds a new dimension to the analysis results that to date has not been reliably captured by the available methods.