Thomas Münzel MD, of Johannes Gutenberg University, sets out the evidence behind traffic noise-induced cardiovascular disease and suggests how it could be mitigated.
The global burden of disease has shifted within the last decades from communicable, maternal, perinatal, and nutritional causes to non-communicable diseases such as atherosclerosis. While medical and scientific efforts have focused primarily on the diagnosis, treatment, and prevention of traditional cardiovascular risk factors (e.g. diabetes, smoking, arterial hypertension, and hyperlipidaemia), recent studies indicate that environmental stressors, including noise and air pollution, may facilitate the development of cardiovascular disease (CVD). Numerous studies have established that traffic noise (road, aircraft, and railway noise) can be associated with increased risk of cardiovascular and metabolic diseases. Until recently, the precise mechanisms underlying noise-induced cardiovascular disease were largely unknown, mainly due to a lack of models for translational research in humans and animals. Noise annoyance and chronic stress, activation of the autonomic and endocrine system, and disturbance of sleep are proposed to ultimately lead to pathophysiologic (vascular) alterations in the intermediate or chronic timeframe contributing directly or indirectly to the initiation and progression of CVD.
The pathophysiology of noise-induced CVD
Noise is any sound that is subjectively unpleasant and disturbing and causes unwanted effects through a direct (auditory such as hearing loss) or indirect (disturbing sleep and communication and sympathetic arousal) pathway. The impact of noise on physiological functions and psychological processes depends on its characteristics, intensity, and nature. Noise pollution in most urban environments originates from transportation (land and air) but may also originate from loudspeakers, sirens, automobile horns, and machinery from industries.
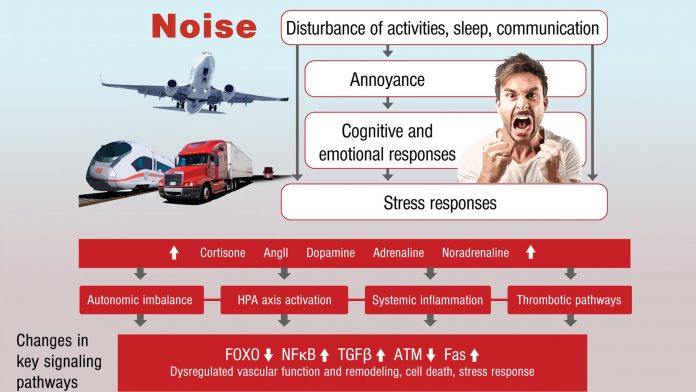
According to the noise reaction model, cardiovascular disease can be caused by noise mainly via an ‘indirect pathway’, where lower levels of noise disturb sleep, communication, and activities, with subsequent emotional and cognitive responses and annoyance (Fig. 2). A resulting chronic stress reaction is proposed to ultimately lead to pathophysiologic alterations in the intermediate or chronic timeframe, which may result in manifest adverse health effects. Furthermore, chronic stress may also generate cardiovascular risk factors on its own, including increased blood pressure, glucose levels, blood viscosity, and blood lipids, and activation of blood coagulation, which may ultimately lead to manifest CVD. Interestingly, emotional stress induced by night-time aircraft noise exposure has been associated with stress cardiomyopathy (TAKOTSUBO-syndrome), a phenomenon which has been linked to excessive stress hormone release. Noise-induced annoyance has been proposed to act as an important effect modifier of the relationship between noise exposure and arterial hypertension and ischaemic coronary artery disease. In addition, high levels of environmental noise have been associated with mental health problems such as depression and anxiety – conditions that are known to adversely affect cardiovascular function.
The molecular mechanisms behind the association between noise and vascular damage and cardiovascular disease are not completely understood. It has been proposed that chronic stress reactions, by activation of the autonomic nervous system and increased levels of circulating cortisol (see above), may lead to vascular (endothelial) dysfunction, mainly through the induction of oxidative stress and subsequent activation of pro-thrombotic pathways and vascular inflammation (Fig. 2). In addition to endothelial dysfunction, elevated blood pressure, dyslipidaemia, changes in blood glucose levels, and altered heart rate variability could contribute to cardiovascular disease development or progression. Importantly, these pathophysiologic mechanisms are potentially not mutually exclusive and may be active at different points in time following noise exposure, as well as varying in importance in relation to chronicity of exposure.
Adverse cardiovascular effects of noise in humans
Translational studies addressing associations between noise and vascular (endothelial) function are rare. In a recent field study, we found that simulated nocturnal aircraft noise was associated with endothelial dysfunction and decreased sleep quality. Importantly, endothelial dysfunction was markedly improved by acute administration of the antioxidant vitamin C, indicating that increased production of reactive oxygen species (ROS) and/or depletion of antioxidant defence significantly contributes to this phenomenon. The associations between noise and endothelial function were found to be substantially more pronounced if the subject had been previously exposed to noise (so-called ‘priming effect’). This indicates that the vasculature is sensitised rather than desensitised to vascular damage in response to repeated noise exposures. Noise-induced vascular dysfunction was found paralleled by increased levels of the stress hormone adrenalin. Furthermore, the negative association between noise and endothelial function was more pronounced in patients with established coronary artery disease. Importantly, no correlation was observed between noise sensitivity or annoyance, suggesting that endothelial function will deteriorate in response to night-time noise, independent of whether there is an annoyance reaction or not. Simulated night-time aircraft noise was also associated with an increase in blood pressure. Thus, our observational studies may explain at least in part the results of studies which found a statistically significant association between night-time aircraft noise and arterial hypertension. Associations between road traffic noise and cardiovascular disease were found to be stronger among people sleeping with open windows or with bedrooms facing the road. Night-time noise interferes with blood pressure and thereby increases cardiovascular risk. Endothelial dysfunction is also established in 24-hour shift workers and in people exposed to chronic sleep restriction, suggesting that night-time noise-induced sleep deprivation and fragmentation may be an important branch on the mechanistic pathway between noise exposure and endothelial dysfunction and cardiovascular disease.
Importantly, endothelial dysfunction has been demonstrated to have prognostic value in patients with peripheral artery disease, arterial hypertension, acute coronary syndrome or chronic stable coronary artery disease. Thus, noise-induced endothelial dysfunction may partly explain the association between transportation noise and CVD found in various epidemiological studies.
Translational studies addressing the adverse cardiovascular effects of noise in animals
Mechanistic studies in animals addressing associations between noise exposure and vascular (endothelial) function and cardiovascular risk are rare. Noise exposure of monkeys (85dB(A), intermittent for nine months) had no effects on the auditory system but significantly increased blood pressure by 30mmHg. Other studies established that white noise exposure of rats for periods of 2-8 weeks (85-100dB(A)) significantly impaired endothelium-dependent vasodilation (measured by acetylcholine in thoracic aorta or mesenteric arterial rings), increased the sensitivity to the vasoconstrictor serotonin, decreased the lumen sizes of micro-vessels, increased systolic blood pressure by 25-37mmHg, and increased circulating markers of oxidative stress.
White noise exposure in the range of 70-100dB(A) has been associated with increased levels of stress hormone, lipid peroxidation, and morphological changes in the heart of rats as well as structural changes of the vasculature that were corrected by the antioxidant vitamin E. Chronic white noise exposure (100dB(A)) also induced an intestinal inflammatory response in rats, with a persistent elevation of IgA, IL-1β, and TNF-α levels. Thus, chronic noise exposure may directly or indirectly regulate gut microbiota-host inflammation homeostasis.
We recently developed an animal model for exposure of mice to aircraft noise events, with a maximum sound pressure level (SPL) of 83dB(A) and a mean SPL of 72dB(A). We aimed to study the non-auditory effects of noise on the cardiovascular system, inflammation, and oxidative stress. Effects of continuous (24h) aircraft noise exposure for 1-4 days were compared with ‘white noise’ as a control noise exposure, using exactly the same average SPL as for aircraft noise. The key findings were that aircraft noise was associated with increased blood pressure, endothelial dysfunction, reduced vascular nitric oxide formation, increased oxidative stress marker, and increased sensitivity of the vasculature to vasoconstrictors. Importantly, these changes were unique for aircraft noise and not observed in response to white noise exposure (applied in the form of a continuous swoosh), suggesting that the characteristics of the noise stimulus (pattern, frequency, exposure time, and intensity) are important. Next-generation sequencing analysis showed that aortic tissues from aircraft noise-treated animals displayed significant changes of genes partly responsible for the regulation of vascular function, vascular remodelling, and cell death. A summary of the main mechanistic pathways, including gene regulatory networks, is provided in Fig. 2.
Epidemiological evidence on noise and cardiovascular disease
The quantity of epidemiological papers on traffic noise and CVD is rapidly growing, especially in recent years. At the same time, the research quality has increased considerably, with much larger study populations and increased focus on adjustment for air pollution. This has resulted in further evidence of traffic noise as a risk factor for major cardiovascular outcomes, such as coronary heart disease, and indicated that traffic noise may also be associated with major cardiovascular disease not investigated previously in a noise context.
Noise and cardiovascular disease
Since the publication of the first study in the late 1980s, the association between traffic noise and coronary heart disease has been studied extensively. Recent meta-analyses consistently conclude that traffic noise is associated with an increased risk of coronary heart disease. The most recent meta-analysis from 2015 included studies on road traffic and aircraft noise, and found a 6% significant increase in risk for every 10dB(A) increase in traffic noise (LDEN), starting as low as 50dB(A). Importantly, the meta-analysis applied strict quality criteria with regard to design, including only incident studies. The meta-analysis also found that the increase in risk remained relatively unchanged after excluding studies that did not account for smoking habits, indicating that lifestyle factors may not always be strong confounders in studies of traffic noise and CVD. Also, cohort studies with full adjustment for socioeconomic status, lifestyle, and air pollution generally find noise to be significantly associated with coronary heart disease. Although house prices are known to be negatively associated with traffic noise, studies have indicated that the association between traffic noise and socioeconomic status may not always be pronounced, as living in city centres of the large metropolitans is popular, attracting residents with high socioeconomic status. A large cohort study found a 14% significant higher risk of incident stroke for every 10dB(A) increase in road traffic noise (LDEN). As for coronary heart disease, this risk increase was independent of adjustment for air pollution. This result was later confirmed by two large studies from London on aircraft and road traffic noise. Both daytime and night-time aircraft noise above 55dB(A) significantly increased risk for stroke hospitalisation with, respectively, 8% and 29% when compared with levels below 50dB(A) in a population of 3.6 million people living around Heathrow Airport, which suggests that night-time noise may be especially hazardous. Similarly, based on 8.6 million residents of London, road traffic noise was found to significantly increase risk for stroke hospitalisation. In further support, recent large population-based studies showed that traffic noise from both roads and aircrafts was associated with higher stroke mortality. Two studies have addressed different sub-types of stroke, and both found traffic noise to be associated with ischaemic stroke and not haemorrhagic stroke, which is as expected given the potential mechanisms.
Traffic noise may also result in heart failure and atrial fibrillation. Two large population studies of 0.75 and 4.41 million persons, respectively, found both road traffic and aircraft noise to significantly increase risk for heart failure, ranging from 2-7% increase in risk per 10dB(A) rise, depending on study and type of exposure. Furthermore, one study found that road traffic noise increased risk for incident atrial fibrillation with 6% for every 10dB(A), although this was not independent of adjustment for air pollution. In addition, we established that annoyance to noise ‘doses-dependently’ increases the prevalence of atrial fibrillation in the Gutenberg Health Study Cohort. These findings highlight an important aspect for road traffic and aircraft noise, namely the correlation with air pollution.
Noise and cardiovascular risk factors
The most comprehensively studied risk factor for cardiovascular disease in a noise context is arterial hypertension. A meta-analysis of 24 studies showed that a 5dB(A) rise in road traffic noise was associated with a significant odds ratio for prevalent hypertension of 1.034. The meta-analysis was based on cross-sectional studies, which limits the interpretation regarding causality. However, studies on incident hypertension are emerging, largely showing that traffic noise is associated with hypertension, thereby supporting the cross-sectional findings. Also, stronger associations with hypertension have been observed for indoor noise as compared with outdoor noise. In further support, a large population study found aircraft, railway, and road traffic noise to be associated with hypertensive heart disease.
Night-time road traffic noise was also found to significantly increase the thoracic aortic calcification burden, a recognised marker of atherosclerosis, and was significantly associated with increased heart rate in a large cohort of 88,000 persons. In addition, the total number of noise events during the night, but not during daytime, has been associated with increased arterial stiffness. Several studies consistently established associations between aircraft and road traffic noise and obesity, a major risk factor for cardiovascular disease, in both cross-sectional and longitudinal studies of high quality. Furthermore, traffic noise was found to significantly increase diabetes risk. As a consequence of stress and sleep disturbance, noise may affect other lifestyle risk factors since traffic noise was demonstrated to be associated with physical inactivity and possibly more smoking and alcohol consumption.
Noise mitigation measures
Noise insulation of buildings is effective at reducing exposure to all outdoor noise sources but is associated with low cost-effectiveness due to high costs of implementation. New technologies and improvements make important contributions to reducing noise levels for all transportation noise sources, e.g. development of quiet engines, low-noise tires for vehicles, and low-noise brake blocks for trains. Road traffic is by far the greatest contributor to traffic noise pollution, and frequently used abatement procedures are reduced speed limits, quiet road surfaces, and noise barriers along major roads. However, due to the extent and the temporal increase in exposure, other strategies like traffic management and regulation and development of low-noise tires are greatly needed. Air transport has increased for many years, and strategies for reducing exposure include restriction or curfews during the night, where noise has been shown to be especially hazardous. However, exposure during morning, daytime and evening are also detrimental to health, and other strategies are needed, e.g. changing the descent procedure and limiting the running of engines on the ground.
Thus, as the percentage of the population exposed to detrimental levels of transportation noise is rising, new developments and legislation to reduce noise are important for public health.
Molecular mechanisms underlying noise-induced vascular damage
Potential (molecular) mechanisms underlying noise-induced cardiovascular disease
Based on the epidemiological evidence and mechanistic insight from translational human and animal data, we propose that noise induces a stress response, characterised by activation of the sympathetic system and increased levels of catecholamines, cortisone and angiotensin-II, which will initiate sequelae, ultimately leading to vascular damage. Angiotensin-II is a potent activator of the vascular and phagocytic NADPH oxidase, which can lead to oxidative stress in the blood and the vasculature. ROS will scavenge nitric oxide (NO) and cause eNOS uncoupling through oxidation of the eNOS cofactor tetrahydrobiopterin and eNOS S-glutathionylation, thereby further increasing vascular oxidative stress. At the level of gene regulation, ROS impair signalling pathways centred around PI3K/Akt, the FOXO transcription factors, TGF-β1 and NF-κB, all of which will lead to activation of the endothelin-1 system, increased levels of circulating interleukin-6 and higher expression of vascular adhesion molecules. Oxidative stress goes hand in hand with increased inflammation. Immune cells (neutrophils, natural killer cells, and monocytes/macrophages) will produce higher amounts of superoxide and NO upon infiltration into the vasculature, ultimately leading to oxidative protein modifications such as 3-nitrotyrosine, malondialdehyde and 4-hydroxynonenal, and adverse redox-regulatory effects on cellular signalling pathways (Fig. 2). Higher circulating and tissue glucocorticoid levels will contribute to a further reduction of endothelial NO production, marked impairment of vasodilation, and increased blood pressure. Constrictive pathways, e.g. expression of endothelin-1 within the vasculature, are activated by the increased levels of stress hormones. The adverse vascular alterations may contribute to the development of arterial hypertension, coronary artery disease, heart failure, and metabolic disorders.
Gaps in the knowledge of noise and air pollution-mediated cardiovascular disease
There are currently no experimental studies that simultaneously have examined the effects of noise and air pollution co-exposure in experimental models or humans. A number of important questions at the mechanistic level in animals may help provide direction for future human studies. The impact of traffic-related air pollutant co-exposure with noise is most worthy of initial study. Finally, the development of technologies that provide personal measures of health in conjunction with data on environmental exposure provides an unprecedented opportunity for research and may allow an extraordinary understanding of the interactions between environmental and non-environmental risk factors.
However, the extent of these advances in knowledge are tempered by the need to manage subject burden and costs and less accurate or precise data due to the inexpensive nature of the devices available for use or reliant on individuals for their proper use.
Summary and conclusions
The presented evidence further strengthens the concept that transportation noise per se contributes to the development of cardiovascular risk of coronary artery disease, arterial hypertension, stroke, and heart failure.
With regard to understanding the pathophysiologic mechanisms, a growing body of evidence finds that noise is associated with oxidative stress, vascular dysfunction, autonomic imbalance, and metabolic abnormalities, not only potentiating the adverse impact of cardiovascular risk factors such as arterial hypertension and diabetes but also contributing to the progression of atherosclerosis and increased susceptibility to cardiovascular events.
Thus, there is increasing rationale for studying the interaction between this novel risk factor and its collective impact on cardio-metabolic diseases. The questions that need to be addressed are many and include the magnitude and time course of response to co-exposure of noise and air pollution, synergistic effects of both exposures on surrogate measures such as blood pressure and metabolic risk, duration of effect/time course of reversal, impact of low-grade background noise exposure on air pollution exposure effects and vice versa, impact of noise on the circadian rhythm, and, finally, the effects on lifestyle (e.g. diet, stress, and exercise).
Perspectives
Clinical competencies and translational implications
Traffic noise is associated with autonomic imbalance, vascular and metabolic abnormalities, and potentiates risk factors such as arterial hypertension and diabetes, which are all mediated, at least in part, by increased oxidative stress. Future prospective clinical trials, but also basic science and translational studies, in people employing various noise sources, such as railway and road traffic noise, have to be performed to more specifically address the pathophysiological consequences of transportation noise on the vasculature, in order to ameliorate the future development of arterial hypertension, coronary artery disease, heart failure, and stroke.
References
- Munzel T et al. The adverse effects of environmental noise exposure on oxidative stress and cardiovascular risk. Antioxid Redox Signal 2018
- Munzel T et al. Environmental Noise and the Cardiovascular System. J Am Coll Cardiol 2018;71:688-697
- Munzel T, Daiber A. Environmental Stressors and Their Impact on Health and Disease with Focus on Oxidative Stress. Antioxid Redox Signal 2018
- Hahad O et al. Annoyance to different noise sources is associated with atrial fibrillation in the Gutenberg Health Study. Int J Cardiol 2018
- Munzel T et al. Environmental stressors and cardio-metabolic disease: part I-epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur Heart J 2017;38:550-556
- Munzel T et al. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J 2017;38:557-564
- Munzel T et al. Effects of noise on vascular function, oxidative stress, and inflammation: mechanistic insight from studies in mice. Eur Heart J 2017;38:2838-2849
- Munzel T et al. Airborne disease: a case of a Takotsubo cardiomyopathie as a consequence of nighttime aircraft noise exposure. Eur Heart J 2016;37:2844
- Schmidt F et al. Nighttime aircraft noise impairs endothelial function and increases blood pressure in patients with or at high risk for coronary artery disease. Clin Res Cardiol 2015;104:23-30
- Schmidt FP et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J 2013;34:3508-3514a
Thomas Münzel MD
Department of Cardiology
University Medical Center Mainz
+49 6131 17 7250
tmuenzel@uni-mainz.de