In healthcare, preventing and controlling healthcare-associated infections (HAIs) is a critical component in ensuring patient safety and optimising clinical outcomes.
These infections, which are not present at the time of a patient’s admission, can develop due to healthcare interventions or contact with the healthcare environment. HAIs pose a significant threat to patient health, increasing morbidity and mortality rates and imposing substantial financial burdens on healthcare systems.
Despite the efficacy of Infection Prevention and Control (IPC) measures, the evolving nature of pathogens and the increasing complexity of medical procedures present ongoing challenges. This discussion explores the multi-faceted approach required to curtail the prevalence of HAIs and the continuous efforts needed to enhance healthcare safety.
What are healthcare-associated infections?
Healthcare-associated infections are infections that patients acquire while receiving treatment for medical or surgical conditions within healthcare facilities. This distinguishes them from community-acquired infections that occur in non-clinical settings.
HAIs generally become evident after 48 hours of hospital admission or within 30 days following a surgical procedure, highlighting their direct connection to healthcare interventions. These infections often involve pathogens that have developed antibiotic resistance, complicating treatment and recovery. In contrast, community-acquired infections arise in environments such as schools or workplaces and may be caused by a broader array of organisms, typically not linked to medical procedures.
In healthcare settings, stringent infection prevention protocols are vital to safeguard patient safety and curtail the transmission routes of HAIs. These measures tackle challenges such as antibiotic-resistant bacteria, ensuring that healthcare environments do not contribute to the escalating issue of resistance.
Implementing these protocols is a cornerstone of patient safety initiatives, as HAIs can spread rapidly among immunocompromised individuals, leading to severe outcomes. Addressing HAIs requires a comprehensive approach that includes diligent hand hygiene, sterile techniques during invasive procedures, and judicious antibiotic use.

Common types of HAIs
Among the most prevalent healthcare-associated infections are respiratory tract infections, surgical site infections, urinary tract infections, bloodstream infections, and gastrointestinal infections. Each presents unique challenges and requires specific control measures, contributing significantly to morbidity and mortality among hospitalised patients.
Key considerations for prevention include:
- Risk factors: Prolonged hospital stays, invasive procedures, compromised immune systems, and the use of devices like ventilators or catheters increase HAI risks
- Transmission routes: HAIs can be transmitted through contact with contaminated surfaces, medical equipment, healthcare personnel, or other patients
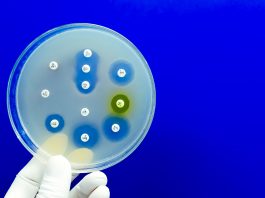
- Antibiotic resistance: Overuse or misuse of antibiotics can lead to resistant bacteria, making HAIs more difficult to treat and control
- Patient outcomes: HAIs can result in longer hospital stays, increased healthcare costs, and higher rates of disability or death.
Effective surveillance methods are key in tracking HAIs and guiding prevention efforts. These methods help identify outbreaks early, monitor infection rate trends, and evaluate the impact of prevention strategies. Ultimately, rigorous adherence to infection control protocols is vital in reducing HAI incidence.
Understanding the connection with sepsis
Understanding the common types of healthcare-associated infections is critical, as these infections significantly heighten the risk of sepsis, a life-threatening condition arising when the body’s response to an infection injures its own tissues and organs. When pathogens from HAIs invade the bloodstream or other parts of the body, the immune system’s aggressive response can lead to widespread inflammation and severe organ dysfunction.
Without proper infection control measures, HAIs can lead to prolonged hospital stays, elevated healthcare costs, and increased strain on medical infrastructure. Antibiotic resistance compounds this issue, as resistant bacterial strains make infections more difficult to treat, further increasing sepsis risks. Ineffective infection control can result in outbreaks that exacerbate individual cases and overall healthcare management challenges.
To effectively reduce HAIs and sepsis, healthcare providers must rigorously enforce hand hygiene protocols and maintain a clean hospital environment. Key strategies include:
- Hand hygiene: Frequent and proper handwashing or using alcohol-based hand sanitisers to reduce pathogen spread
- Antibiotic stewardship: Judicious use of antibiotics to prevent the emergence of resistant bacterial strains and preserve current treatments’ effectiveness
- Cohort screening: Identifying and separating infected or colonised patients to prevent cross-transmission among patients and healthcare staff
- Surveillance strategies: Consistent monitoring of infection rates and types to quickly identify and respond to outbreaks
These measures, when diligently applied, improve compliance across the healthcare system. Educating healthcare workers on the importance of these measures, combined with consistent monitoring and feedback, helps maintain high standards of care and patient safety.
Current research
Research on avoiding and treating healthcare-associated infections focuses on enhancing infection prevention protocols, developing efficient surveillance systems, and combating antimicrobial resistance. Investigators delve into the epidemiology of HAIs to understand prevalence rates across different economies, tailoring global strategies for infection control. These strategies reinforce hand hygiene, environmental cleanliness, and the judicious use of antibiotics through stewardship programmes.
Efforts to address antimicrobial resistance, a significant threat to current treatment effectiveness and HAI control, are paramount. Developing new antimicrobials and managing existing ones are areas of intense investigation. Researchers are also refining surveillance protocols to reliably track various HAIs’ incidence, enabling healthcare facilities to respond swiftly and effectively to emerging infection patterns.
By examining specific preventive measures, including optimising hand hygiene practices, cohorting patients based on infection status, and implementing targeted antibiotic stewardship interventions, research endeavours aim to establish robust and evidence-based practices universally adopted to minimise HAI risks and impacts.
Preventing and controlling HAIs is a multi-faceted challenge requiring continuous efforts, rigorous protocols, and ongoing research to ensure patient safety and improve healthcare quality.